Volume 20, Issue 2 (10-2023)
J Res Dev Nurs Midw 2023, 20(2): 39-43 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadi Sangsari A, Roohi G, Sabzi Z, Abdollahi A A, Behnampour N. A comparison of Cardiac Triage Method and Emergency Severity Index impact on admission time for acute coronary syndrome patients. J Res Dev Nurs Midw 2023; 20 (2) :39-43
URL: http://nmj.goums.ac.ir/article-1-1293-en.html
URL: http://nmj.goums.ac.ir/article-1-1293-en.html
1- School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran
2- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,roohi_43@yahoo.com
3- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran
2- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,
3- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran
Full-Text [PDF 565 kb]
(2130 Downloads)
| Abstract (HTML) (3779 Views)
Full-Text: (745 Views)
Introduction
Triage is a hierarchical decision-making process that categorizes patients based on the severity and acuteness of their condition compared to other patients. It is one of the most critical management activities in providing healthcare services in the emergency department (1). All individuals seeking care in the emergency department are triaged to identify critically ill patients based on the severity of their condition (2). One common reason patients visit hospital emergency departments is acute coronary syndrome, a life-threatening condition (3). Therefore, the rapid and accurate identification of these patients is paramount, as undiagnosed cases can lead to a high mortality rate and were the largest source of negligence claims in emergency departments (4). On the other hand, precise and efficient triage for chest pain presents a healthcare challenge (5).
The primary objective of triage is the rapid identification of patients with critical conditions, time sensitivity, and prioritizing their care over individuals who can wait (1). In this context, the accuracy and reliability of triage in the emergency department are of utmost importance. Under-triaging or failing to distinguish patients with severe acute illnesses (such as myocardial infarction and sepsis) from those with less urgent needs (such as gastrointestinal issues and localized infections) can lead to delays in time-sensitive interventions, clinical severity, complications, and patient mortality (1).
One of the most widely used triage tools in emergency departments worldwide is the Emergency Severity Index (ESI) five-level triage. This system has also been adopted in our country (6). Various studies that have employed the standard triage scale have shown the presence of various errors in triage (1,7). Despite its widespread acceptance and many strengths, such as ease of use and its correlation with predicting available resources in the emergency department, ESI triage has limitations, including a heavy reliance on the clinical judgment of the triage personnel, challenges in resource allocation, limited precision, and low accuracy in classifying patients with suspected acute coronary syndrome (1).
The question of how effective triage scales are in correctly identifying critically ill patients remains debatable. Fazl Asgharpour et al. have demonstrated that the ESI, which provides non-specialized and general triage criteria for all types of patients, may not adequately identify patients with complaints of chest pain, as a significant constraint in this matter is that the ESI triage scale may not be able to identify subgroups of patients (8) accurately. Determining triage levels is often associated with tracking patients in specific care areas, especially in designated emergency departments (9).
In emergencies, every second and minute counts for a patient, and these moments can make the difference between life and severe disability or even life and death. Moreover, making precise triage decisions is of utmost importance because accurate triage can significantly reduce mortality rates, whereas errors in this decision-making process can seriously jeopardize a patient's life (10). However, this relies on the triage nurse's ability to establish a mental connection between the patient's condition and the risk of cardiac failure. As demonstrated by the study's findings by Fazl Asghari et al., a specific triage for cardiac patients can reduce the time required for assessment and intervention in cardiac cases (8).
Furthermore, a study by Pouyanmehr et al. revealed that the resource consumption among hospitalized patients with heart failure who were triaged based on the ESI scale was significantly lower than those who received an emergency severity index (11). Given that the rapid admission of patients is crucial for successful emergency department operation (12), and considering the lack of a global consensus on patient triage (13), cardiac patient triage must be conducted as quickly and precisely as possible.
Hence, recognizing the importance of triage, especially for cardiac patients, and the availability of a specialized triage method for them, this study was conducted to compare the implementation of two triage methods, cardiac triage and ESI, on the admission time of patients suffering from acute coronary syndrome at the educational and medical center.
Methods
This interventional study was conducted in 2019-2020 on patients presenting to the triage unit of the Emergency Department at Shahid Sayad Shirazi Educational and Medical Center in Gorgan, located in northern Iran. The inclusion criteria for the study were patients aged 18 to 85 presenting to the emergency department with complaints of chest pain and shortness of breath and no history of chest trauma.
Based on the study by Asghar Pour et al. (8), with a confidence level of 95% and a test power of 90%, the mean in the first group was 22.0 ± 0.0, and in the second group was 10.0 ± 0.0.
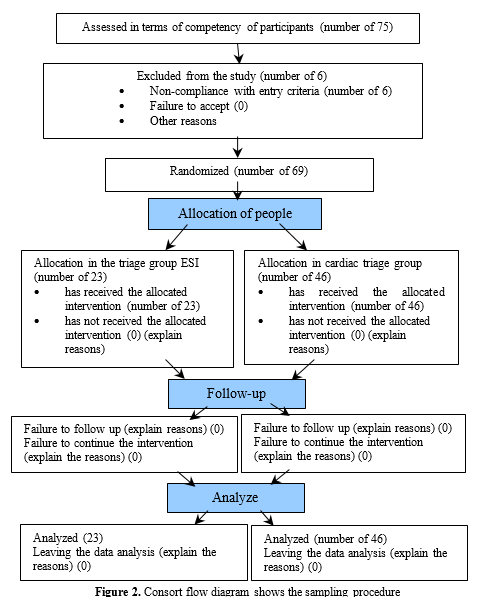
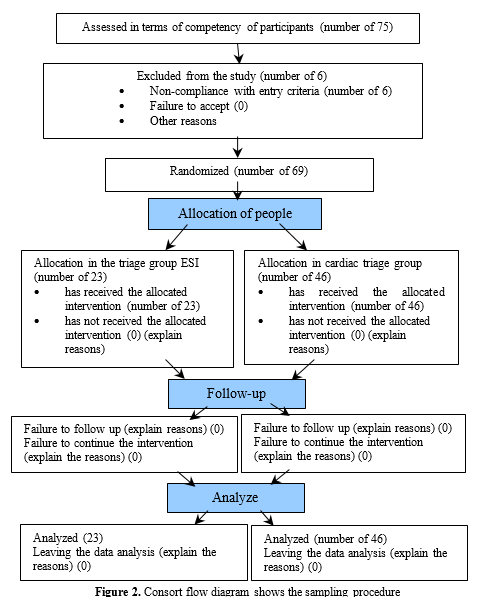
According to the sample size formula, each group required 31 individuals, totaling 62 samples. However, due to unequal variances (standard deviations) in the two groups, the sample size should be based on a 2:1 ratio (R=2) in the group with the more considerable variance. Consequently, the total sample size increased to 69 patients, with 46 individuals in the intervention group and 23 in the control group.
The researcher performed sampling in the triage room during three shifts: morning, afternoon, and night. Initially, all patients meeting the inclusion criteria were randomly assigned to either the control or intervention group using a simple random allocation method, achieved by tossing a coin (heads or tails). In this study, patients in the control group were triaged based on the ESI scale, while patients in the intervention group were triaged using the Cardiac Triage Scale. The study was conducted with one group of patients unaware of their assigned study group, ensuring fairness in the research process.
Before patients were enrolled in the research, written informed consent for participation in the study was obtained from them. In case of incapacitation, consent was obtained from the patient's legal guardian and the attending physician. To this end, during the examination and history-taking process, the research objectives were explained to the patient and their family in the shortest possible time. If the patient expressed a willingness to participate, they were enrolled in the study.
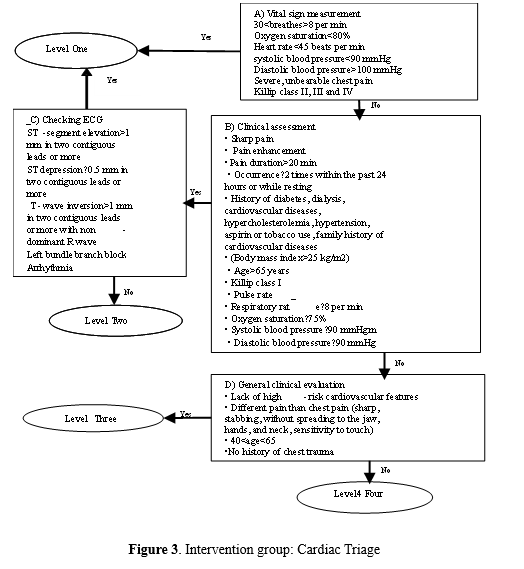
In the intervention group, patients underwent the following stages of heart triage (Figure 1) from the time of admission to the emergency department until admission to the ward or discharge: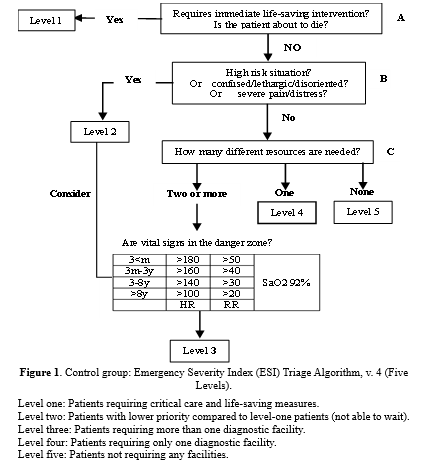
Additionally, in the patient control group, routine screening was performed in the emergency department using the ESI based on guidelines provided by the Ministry of Health (Figure 2). This index, designed for the first time in the United States, categorizes patients into five levels based on the severity of their illness and the facilities required (8). Its validity and reliability have been confirmed and are commonly employed by the Ministry of Health, Treatment, and Medical Education.
According to this form, the researcher triages patients based on the severity of their illness and the facilities required. The severity of the illness is determined based on life-threatening factors, risk symptoms, and vital signs. The second criterion is determined based on the researcher's experience, and patients are categorized into five levels.
This study used a form for recording personal characteristics and temporal indices, a cardiac triage scale, and an ESI triage scale. These included temporal indices such as the duration from admission to triage room exit, the duration of the first visit by a general practitioner, the time it takes for a physician's order to be checked by a nurse, the duration of being under observation, the duration of the first visit by a specialist physician, the duration of patient discharge from the emergency department, patient mortality, and the time of the first ECG recording in two groups. This study used this form to assess vital signs using a monitoring device with a blood pressure cuff and pulse oximeter manufactured by VECTRA and an automatic ECG machine manufactured by Nihon Kohden, model ECG2150, from China. (Figure 3).
The data were described using central tendency and dispersion indices (mean and standard deviation) and frequency distribution tables. Additionally, the normality of the distribution of quantitative variables (systolic blood pressure, diastolic blood pressure, pulse rate, respiratory rate, arterial oxygen saturation, age, and mean temporal indices in intervention and control groups) was assessed using the Shapiro-Wilk test. Based on the normality status, the Mann-Whitney test was employed to compare these characteristics between the two groups. For data analysis, SPSS statistical software version 18 was utilized.
Results
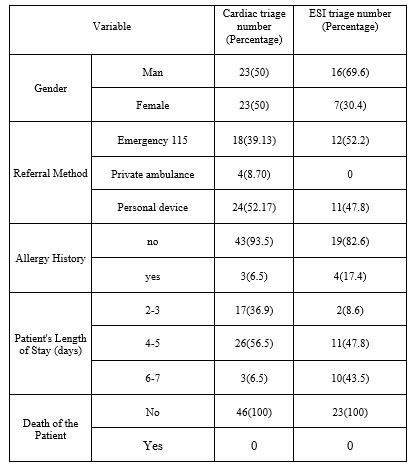
In this study, 75 individuals were initially enrolled, with 6 participants who did not meet the entry criteria being subsequently excluded. Thus, 69 patients, all suffering from acute coronary syndrome in Gorgan and complaining of symptoms such as shortness of breath and chest pain, were ultimately included in the study. The study's results indicated that in the cardiac triage group, the gender distribution was equal between males and females. However, in the ESI triage group, there was a higher proportion of male participants, comprising 16 individuals, which accounted for 69.6% of the group.
When analyzing the mode of transportation to the hospital, it was observed that in the intervention group, the majority of patients arrived using personal vehicles, which accounted for 24 individuals, constituting 52.17% of the group. Conversely, in the control group, most referrals were made through emergency services 115, with 12 individuals representing 52.2% of the group.
Regarding hospitalization duration, more than half of the patients in the intervention group, precisely 26 individuals or 56.5%, were hospitalized for a period ranging from 4 to 5 days. On the other hand, in the control group, patients were typically hospitalized for an average duration of 4 to 7 days.
The mean age of participants in the cardiac triage group was calculated to be 49.58 ± 16.58, while in the ESI triage group, it was 51.06 ± 8.55, as shown in Table 1..
The Shapiro-Wilk test revealed that the data follows a normal distribution in the ESI triage group. However, the data did not exhibit a normal distribution in the cardiac triage group. Therefore, the Mann-Whitney test was used for data analysis.
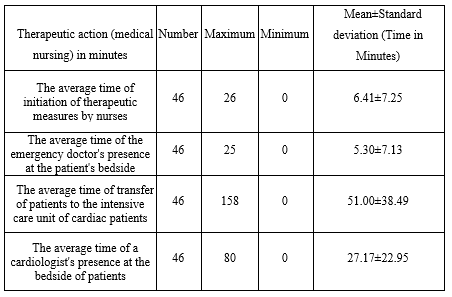
The findings indicated that, on average, patients in the cardiac triage group wait approximately 6.41 minutes for triage to be conducted. This average ranged from immediate triage without delay to a maximum of 26 minutes. In the cardiac triage group, it takes 5.30 minutes for the emergency physician to visit the patient. The average time for patients to be transferred to the cardiac intensive care unit in the cardiac triage group is 51 minutes. This average ranged from immediate transfer without delay to a maximum of 158 minutes. Furthermore, on average, in the cardiac triage group, it takes 27.17 minutes for the cardiology specialist to be present at the patient's bedside. This average ranged from immediate presence without delay to a maximum of 80 minutes (refer to Table 2).
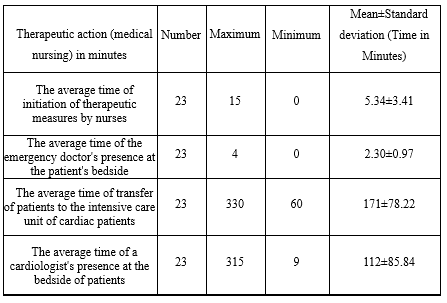
The findings reveal that, on average, nurses initiated therapeutic actions for patients in the ESI 5.34 triage group within 5 minutes. This average spanned from immediate initiation of therapeutic actions by nurses to a maximum of 15 minutes without delay. Additionally, the average duration of emergency physicians at the bedside of patients in the ESI triage group was 2.30 minutes. This average ranged from an immediate presence of emergency physicians at the bedside to a maximum of 4 minutes without delay.
Furthermore, the average time for patient transfer to the cardiac intensive care unit in the ESI triage group was 171.47 minutes. This average ranged from 60 minutes to a maximum of 330 minutes for the transfer duration. On average, cardiac specialist physicians spent 112.39 minutes at the bedside of patients in the ESI triage group (Table 3).
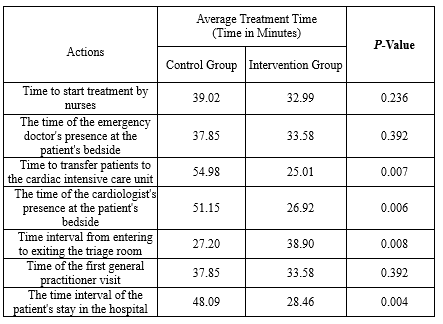
The findings reveal significant differences in transfer times between the two groups, as determined by the Whitney test, from the emergency department to the cardiac intensive care unit. This difference is most pronounced in the cardiac triage group, where patients are expedited to the cardiac intensive care unit using the cardiac triage approach in a shorter period (p < 0.007). Furthermore, the results indicate a significant difference in the two groups' average time a cardiac specialist physician spends with patients at the bedside. In the cardiac triage group, utilizing the cardiac triage method, this average is shorter, and the first visit by the cardiac specialist occurs more promptly (p < 0.006).
Similarly, based on the Whitney test, there is a notable difference in the meantime interval between admission and discharge from the triage room between the two groups. This mean interval is longer in the cardiac triage group, where more comprehensive assessments are conducted during triage using the cardiac triage method, resulting in an extended duration (p = 0.008).
In this context, the results of this study indicate a significant difference in the mean hospitalization duration for patients in the two groups, as assessed by the Whitney test. This mean duration is shorter in the cardiac triage group using the cardiac triage approach (p < 0.004) (Table 4).
Discussion
The findings demonstrate that therapeutic interventions and specialist physician visits occurred more promptly in the cardiac triage group. This finding is in line with the dynamic study results of Mehri et al. (11). Similarly, Hughes et al. (2018) in Australia revealed that timely electrocardiogram (ECG) recording is a crucial and impactful indicator of quality care in cardiac patients, as the time interval from patient admission to ECG acquisition is a pivotal aspect of the treatment process (14). Ho et al. also demonstrated that the specific triage method for cardiac patients is more reliable than the conventional approach (15). Furthermore, Frisoli et al. 2017 indicated that while exercise testing may prolong patients' hospital stays, it offers a more precise diagnostic method for cardiac diseases (16). Therefore, despite its broader scope for patients, the cardiac triage approach can be more beneficial in diagnosing and treating patients with acute coronary syndrome.
The findings indicate that in the ESI triage group, nurses initiated therapeutic actions more quickly on average. These findings do not align with the results of the study by Asgharpour et al. (8) and Alizadeh et al., where they reported an average time interval from admission to the administration of thrombolytic drugs for patients as 31.8 minutes (17). A potential reason for this disparity in findings could be attributed to the study type and differences in the physical infrastructure of hospitals.
The study results also reveal that in the cardiac triage group, patients were transferred to the cardiac intensive care unit in a shorter period. This finding is consistent with the results of the study conducted by Mirhaghi et al. in 2018, where they also showed that the time interval from admission to ECG performance for cardiac failure patients in the triage group was less than that in the ESI group (18). Furthermore, this finding aligns with the results of the Asgharpour et al. study (8), which suggests that a more precise assessment of cardiac triage procedures can expedite the decision-making process for patient transfer to the treatment team.
Moreover, based on the current study's results, the presence of a cardiology specialist physician at the patient's bedside in the cardiac triage group occurred more rapidly. This finding contrasts with a study by Pouyamehr et al. (2019), which demonstrated that the timing of visits by cardiology physicians did not significantly differ between the cardiac failure triage and ESI triage methods (11). Differences in the underlying disease, variations in the workload of specialized physicians in different hospitals, and the type of triage may be potential reasons for differences in the study outcomes.
The findings of this research indicate a significant difference in the average time from admission to discharge from the triage room between the two groups. This finding is consistent with the dynamic studies conducted by Pouyamehr et al. (11), and Bohalla et al. (19). Another result of this study is the difference in the average length of hospitalization in the two groups, with a significantly shorter duration of hospitalization for patients in the cardiac triage group compared to the ESI triage group. These findings align with those of Gharaei et al., who reported that ESI triage did not accurately predict the occurrence of cardiac problems. Patients in the ESI triage group experienced an extended rehospitalization period due to cardiac issues after discharge, which exceeded two weeks (20). Consistent with the findings of the present study, Bohalla et al. (2019) also demonstrated that the average duration of hospitalization in the intensive care unit for individuals with ACS due to maintaining triage was 1.6 days, as opposed to 2.8 days for those triaged in the regular care unit for treatment (19).
Conclusion
The results of this study demonstrate that the implementation of the cardiac triage scale has positively impacted the time-based triage indicators for patients in the emergency department. Its adoption is crucial for reducing response times and facilitating therapeutic interventions for these patients. Therefore, we strongly recommend providing training and implementing this scale for nurses working in hospital emergency departments when dealing with cardiac emergency patients. Additionally, it is essential to note that the differences in patient assessment methods between the two groups may affect the subsequent outcomes of the patients, which constitutes a limitation of this study.
Acknowledgement
This study is based on the master's thesis of a critical care nursing student at the School of Nursing and Midwifery, Golestan University of Medical Sciences. The authors thank the Research and Technology Deputy of Golestan University of Medical Sciences for their invaluable spiritual and financial support for this research project (and thesis). We also express our sincere appreciation to the nurses who collaborated in this study and to all the patients who presented to the emergency center of Gorgan Educational-Medical Center and participated in the study.
Funding sources
This research has been supported and funded by the Golestan University of Medical Sciences, Gorgan, Iran (project code: 110902).
Ethical statement
This protocol study has been approved by the Research Ethics Committee of Golestan University of Medical Sciences (Ethical code: IR.GOUMS.REC.1398.222).
Conflicts of interest
the authors declare that there is no conflict of interest.
Author contributions
All authors have contributed significantly to this study. Mohammadi and Roohi designed the project, performed the data collection and wrote the manuscript, Behnampour analyzed data, Sabzi and Abdollahi were scientific advisers of the project and participated in data collection, Roohi also supervised the study. All the authors approved the content of the manuscript.
Triage is a hierarchical decision-making process that categorizes patients based on the severity and acuteness of their condition compared to other patients. It is one of the most critical management activities in providing healthcare services in the emergency department (1). All individuals seeking care in the emergency department are triaged to identify critically ill patients based on the severity of their condition (2). One common reason patients visit hospital emergency departments is acute coronary syndrome, a life-threatening condition (3). Therefore, the rapid and accurate identification of these patients is paramount, as undiagnosed cases can lead to a high mortality rate and were the largest source of negligence claims in emergency departments (4). On the other hand, precise and efficient triage for chest pain presents a healthcare challenge (5).
The primary objective of triage is the rapid identification of patients with critical conditions, time sensitivity, and prioritizing their care over individuals who can wait (1). In this context, the accuracy and reliability of triage in the emergency department are of utmost importance. Under-triaging or failing to distinguish patients with severe acute illnesses (such as myocardial infarction and sepsis) from those with less urgent needs (such as gastrointestinal issues and localized infections) can lead to delays in time-sensitive interventions, clinical severity, complications, and patient mortality (1).
One of the most widely used triage tools in emergency departments worldwide is the Emergency Severity Index (ESI) five-level triage. This system has also been adopted in our country (6). Various studies that have employed the standard triage scale have shown the presence of various errors in triage (1,7). Despite its widespread acceptance and many strengths, such as ease of use and its correlation with predicting available resources in the emergency department, ESI triage has limitations, including a heavy reliance on the clinical judgment of the triage personnel, challenges in resource allocation, limited precision, and low accuracy in classifying patients with suspected acute coronary syndrome (1).
The question of how effective triage scales are in correctly identifying critically ill patients remains debatable. Fazl Asgharpour et al. have demonstrated that the ESI, which provides non-specialized and general triage criteria for all types of patients, may not adequately identify patients with complaints of chest pain, as a significant constraint in this matter is that the ESI triage scale may not be able to identify subgroups of patients (8) accurately. Determining triage levels is often associated with tracking patients in specific care areas, especially in designated emergency departments (9).
In emergencies, every second and minute counts for a patient, and these moments can make the difference between life and severe disability or even life and death. Moreover, making precise triage decisions is of utmost importance because accurate triage can significantly reduce mortality rates, whereas errors in this decision-making process can seriously jeopardize a patient's life (10). However, this relies on the triage nurse's ability to establish a mental connection between the patient's condition and the risk of cardiac failure. As demonstrated by the study's findings by Fazl Asghari et al., a specific triage for cardiac patients can reduce the time required for assessment and intervention in cardiac cases (8).
Furthermore, a study by Pouyanmehr et al. revealed that the resource consumption among hospitalized patients with heart failure who were triaged based on the ESI scale was significantly lower than those who received an emergency severity index (11). Given that the rapid admission of patients is crucial for successful emergency department operation (12), and considering the lack of a global consensus on patient triage (13), cardiac patient triage must be conducted as quickly and precisely as possible.
Hence, recognizing the importance of triage, especially for cardiac patients, and the availability of a specialized triage method for them, this study was conducted to compare the implementation of two triage methods, cardiac triage and ESI, on the admission time of patients suffering from acute coronary syndrome at the educational and medical center.
Methods
This interventional study was conducted in 2019-2020 on patients presenting to the triage unit of the Emergency Department at Shahid Sayad Shirazi Educational and Medical Center in Gorgan, located in northern Iran. The inclusion criteria for the study were patients aged 18 to 85 presenting to the emergency department with complaints of chest pain and shortness of breath and no history of chest trauma.
Based on the study by Asghar Pour et al. (8), with a confidence level of 95% and a test power of 90%, the mean in the first group was 22.0 ± 0.0, and in the second group was 10.0 ± 0.0.
According to the sample size formula, each group required 31 individuals, totaling 62 samples. However, due to unequal variances (standard deviations) in the two groups, the sample size should be based on a 2:1 ratio (R=2) in the group with the more considerable variance. Consequently, the total sample size increased to 69 patients, with 46 individuals in the intervention group and 23 in the control group.
The researcher performed sampling in the triage room during three shifts: morning, afternoon, and night. Initially, all patients meeting the inclusion criteria were randomly assigned to either the control or intervention group using a simple random allocation method, achieved by tossing a coin (heads or tails). In this study, patients in the control group were triaged based on the ESI scale, while patients in the intervention group were triaged using the Cardiac Triage Scale. The study was conducted with one group of patients unaware of their assigned study group, ensuring fairness in the research process.
Before patients were enrolled in the research, written informed consent for participation in the study was obtained from them. In case of incapacitation, consent was obtained from the patient's legal guardian and the attending physician. To this end, during the examination and history-taking process, the research objectives were explained to the patient and their family in the shortest possible time. If the patient expressed a willingness to participate, they were enrolled in the study.
In the intervention group, patients underwent the following stages of heart triage (Figure 1) from the time of admission to the emergency department until admission to the ward or discharge:
- Upon arrival at the emergency department, patients were assessed based on "criteria A," which included the following vital signs: respiratory rate less than 30 breaths per minute and more than 8 breaths per minute, arterial blood oxygen saturation above 80%, heart rate exceeding 45 beats per minute, systolic blood pressure between 90 to 180 mmHg, and diastolic blood pressure exceeding 100 mmHg. Severe, intolerable chest pain and classification into Killip class 2, 3, or 4 were determined based on the patient's clinical symptoms, reflecting the patient's current status and pre-notification.
- Class 1, in which no added sounds are heard in the patient's lungs, and there is no S3 gallop. The patient's pre-notification is good, with a mortality rate of less than 5%.
- Class 2, in which the S3 gallop sound is heard in the heart, or moist rales are heard at the lung bases. The mortality rate is approximately 25%.
- Class 3, in which the S3 gallop sound is present, moist rales are heard in more than half of the lungs. Mortality rates range from 50% to 60%.
- Class 4, where the patient exhibits signs of cardiogenic shock, with mortality rates ranging from 90% to 100% (8).
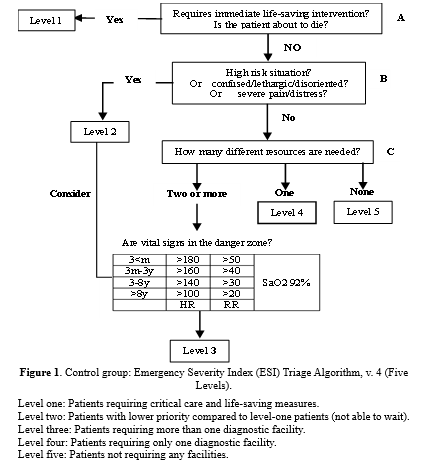
Additionally, in the patient control group, routine screening was performed in the emergency department using the ESI based on guidelines provided by the Ministry of Health (Figure 2). This index, designed for the first time in the United States, categorizes patients into five levels based on the severity of their illness and the facilities required (8). Its validity and reliability have been confirmed and are commonly employed by the Ministry of Health, Treatment, and Medical Education.
According to this form, the researcher triages patients based on the severity of their illness and the facilities required. The severity of the illness is determined based on life-threatening factors, risk symptoms, and vital signs. The second criterion is determined based on the researcher's experience, and patients are categorized into five levels.
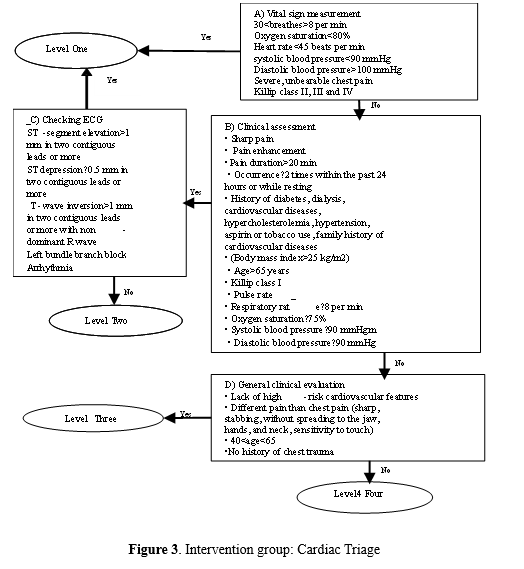
This study used a form for recording personal characteristics and temporal indices, a cardiac triage scale, and an ESI triage scale. These included temporal indices such as the duration from admission to triage room exit, the duration of the first visit by a general practitioner, the time it takes for a physician's order to be checked by a nurse, the duration of being under observation, the duration of the first visit by a specialist physician, the duration of patient discharge from the emergency department, patient mortality, and the time of the first ECG recording in two groups. This study used this form to assess vital signs using a monitoring device with a blood pressure cuff and pulse oximeter manufactured by VECTRA and an automatic ECG machine manufactured by Nihon Kohden, model ECG2150, from China. (Figure 3).
The data were described using central tendency and dispersion indices (mean and standard deviation) and frequency distribution tables. Additionally, the normality of the distribution of quantitative variables (systolic blood pressure, diastolic blood pressure, pulse rate, respiratory rate, arterial oxygen saturation, age, and mean temporal indices in intervention and control groups) was assessed using the Shapiro-Wilk test. Based on the normality status, the Mann-Whitney test was employed to compare these characteristics between the two groups. For data analysis, SPSS statistical software version 18 was utilized.
Results
In this study, 75 individuals were initially enrolled, with 6 participants who did not meet the entry criteria being subsequently excluded. Thus, 69 patients, all suffering from acute coronary syndrome in Gorgan and complaining of symptoms such as shortness of breath and chest pain, were ultimately included in the study. The study's results indicated that in the cardiac triage group, the gender distribution was equal between males and females. However, in the ESI triage group, there was a higher proportion of male participants, comprising 16 individuals, which accounted for 69.6% of the group.
When analyzing the mode of transportation to the hospital, it was observed that in the intervention group, the majority of patients arrived using personal vehicles, which accounted for 24 individuals, constituting 52.17% of the group. Conversely, in the control group, most referrals were made through emergency services 115, with 12 individuals representing 52.2% of the group.
Regarding hospitalization duration, more than half of the patients in the intervention group, precisely 26 individuals or 56.5%, were hospitalized for a period ranging from 4 to 5 days. On the other hand, in the control group, patients were typically hospitalized for an average duration of 4 to 7 days.
The mean age of participants in the cardiac triage group was calculated to be 49.58 ± 16.58, while in the ESI triage group, it was 51.06 ± 8.55, as shown in Table 1..
|
Table 1. Individual characteristics of patients with acute coronary syndrome in cardiac triage and ESI triage groups
 |
The findings indicated that, on average, patients in the cardiac triage group wait approximately 6.41 minutes for triage to be conducted. This average ranged from immediate triage without delay to a maximum of 26 minutes. In the cardiac triage group, it takes 5.30 minutes for the emergency physician to visit the patient. The average time for patients to be transferred to the cardiac intensive care unit in the cardiac triage group is 51 minutes. This average ranged from immediate transfer without delay to a maximum of 158 minutes. Furthermore, on average, in the cardiac triage group, it takes 27.17 minutes for the cardiology specialist to be present at the patient's bedside. This average ranged from immediate presence without delay to a maximum of 80 minutes (refer to Table 2).
|
Table 2. Average time for medical and nursing interventions for patients with acute coronary syndrome in the cardiac triage group.
 |
Furthermore, the average time for patient transfer to the cardiac intensive care unit in the ESI triage group was 171.47 minutes. This average ranged from 60 minutes to a maximum of 330 minutes for the transfer duration. On average, cardiac specialist physicians spent 112.39 minutes at the bedside of patients in the ESI triage group (Table 3).
|
Table 3. Average duration of therapeutic actions (Medical and Nursing) for patients with acute coronary syndrome in the ESI triage group
 |
Similarly, based on the Whitney test, there is a notable difference in the meantime interval between admission and discharge from the triage room between the two groups. This mean interval is longer in the cardiac triage group, where more comprehensive assessments are conducted during triage using the cardiac triage method, resulting in an extended duration (p = 0.008).
In this context, the results of this study indicate a significant difference in the mean hospitalization duration for patients in the two groups, as assessed by the Whitney test. This mean duration is shorter in the cardiac triage group using the cardiac triage approach (p < 0.004) (Table 4).
|
Table 4. Comparison of the average time of treatment procedures (Medical and Nursing) for patients with acute coronary syndrome in two groups of cardiac triages and ESI
 |
The findings demonstrate that therapeutic interventions and specialist physician visits occurred more promptly in the cardiac triage group. This finding is in line with the dynamic study results of Mehri et al. (11). Similarly, Hughes et al. (2018) in Australia revealed that timely electrocardiogram (ECG) recording is a crucial and impactful indicator of quality care in cardiac patients, as the time interval from patient admission to ECG acquisition is a pivotal aspect of the treatment process (14). Ho et al. also demonstrated that the specific triage method for cardiac patients is more reliable than the conventional approach (15). Furthermore, Frisoli et al. 2017 indicated that while exercise testing may prolong patients' hospital stays, it offers a more precise diagnostic method for cardiac diseases (16). Therefore, despite its broader scope for patients, the cardiac triage approach can be more beneficial in diagnosing and treating patients with acute coronary syndrome.
The findings indicate that in the ESI triage group, nurses initiated therapeutic actions more quickly on average. These findings do not align with the results of the study by Asgharpour et al. (8) and Alizadeh et al., where they reported an average time interval from admission to the administration of thrombolytic drugs for patients as 31.8 minutes (17). A potential reason for this disparity in findings could be attributed to the study type and differences in the physical infrastructure of hospitals.
The study results also reveal that in the cardiac triage group, patients were transferred to the cardiac intensive care unit in a shorter period. This finding is consistent with the results of the study conducted by Mirhaghi et al. in 2018, where they also showed that the time interval from admission to ECG performance for cardiac failure patients in the triage group was less than that in the ESI group (18). Furthermore, this finding aligns with the results of the Asgharpour et al. study (8), which suggests that a more precise assessment of cardiac triage procedures can expedite the decision-making process for patient transfer to the treatment team.
Moreover, based on the current study's results, the presence of a cardiology specialist physician at the patient's bedside in the cardiac triage group occurred more rapidly. This finding contrasts with a study by Pouyamehr et al. (2019), which demonstrated that the timing of visits by cardiology physicians did not significantly differ between the cardiac failure triage and ESI triage methods (11). Differences in the underlying disease, variations in the workload of specialized physicians in different hospitals, and the type of triage may be potential reasons for differences in the study outcomes.
The findings of this research indicate a significant difference in the average time from admission to discharge from the triage room between the two groups. This finding is consistent with the dynamic studies conducted by Pouyamehr et al. (11), and Bohalla et al. (19). Another result of this study is the difference in the average length of hospitalization in the two groups, with a significantly shorter duration of hospitalization for patients in the cardiac triage group compared to the ESI triage group. These findings align with those of Gharaei et al., who reported that ESI triage did not accurately predict the occurrence of cardiac problems. Patients in the ESI triage group experienced an extended rehospitalization period due to cardiac issues after discharge, which exceeded two weeks (20). Consistent with the findings of the present study, Bohalla et al. (2019) also demonstrated that the average duration of hospitalization in the intensive care unit for individuals with ACS due to maintaining triage was 1.6 days, as opposed to 2.8 days for those triaged in the regular care unit for treatment (19).
Conclusion
The results of this study demonstrate that the implementation of the cardiac triage scale has positively impacted the time-based triage indicators for patients in the emergency department. Its adoption is crucial for reducing response times and facilitating therapeutic interventions for these patients. Therefore, we strongly recommend providing training and implementing this scale for nurses working in hospital emergency departments when dealing with cardiac emergency patients. Additionally, it is essential to note that the differences in patient assessment methods between the two groups may affect the subsequent outcomes of the patients, which constitutes a limitation of this study.
Acknowledgement
This study is based on the master's thesis of a critical care nursing student at the School of Nursing and Midwifery, Golestan University of Medical Sciences. The authors thank the Research and Technology Deputy of Golestan University of Medical Sciences for their invaluable spiritual and financial support for this research project (and thesis). We also express our sincere appreciation to the nurses who collaborated in this study and to all the patients who presented to the emergency center of Gorgan Educational-Medical Center and participated in the study.
Funding sources
This research has been supported and funded by the Golestan University of Medical Sciences, Gorgan, Iran (project code: 110902).
Ethical statement
This protocol study has been approved by the Research Ethics Committee of Golestan University of Medical Sciences (Ethical code: IR.GOUMS.REC.1398.222).
Conflicts of interest
the authors declare that there is no conflict of interest.
Author contributions
All authors have contributed significantly to this study. Mohammadi and Roohi designed the project, performed the data collection and wrote the manuscript, Behnampour analyzed data, Sabzi and Abdollahi were scientific advisers of the project and participated in data collection, Roohi also supervised the study. All the authors approved the content of the manuscript.
Type of study: Original Article |
Subject:
Nursing
References
1. Hinson JS, Martinez DA, Schmitz PS, Toerper M, Radu D, Scheulen J, et al. Accuracy of emergency department triage using the Emergency Severity Index and independent predictors of under-triage and over-triage in Brazil: a retrospective cohort analysis. Int J Emerg Med. 2018;11(1):3. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Heravi M, Setayeshi S. Intelligent and fast recognition of heart disease based on synergy of linear neural network and logistic regression model. J Mazandaran Univ Med Sci. 2014;24(112):78-87. [View at Publisher] [Google Scholar]
3. Crim MT, Berkowitz SA, Saheed M, Miller J, Deutschendorf A, Gerstenblith G, Hill P, Korley FK. Novel emergency department risk score discriminates acute coronary syndrome among chest pain patients with known coronary artery disease. Crit Pathw Cardiol. 2016;15(4):138-44. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Šljivo A, Mulać A, Džidić-Krivić A, Ivanović K, Radoičić D, Selimović A, et al. HEART Score and Its Implementation in Emergency Medicine Departments in the West Balkan Region-A Pilot Study. Healthcare (Basel). 2023;11(17):2372. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Raff GL, Hoffmann U, Udelson JE. Trials of imaging use in the emergency department for acute chest pain. JACC Cardiovasc Imaging. 2017;10(3):338-49. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Gilboy N, Tanabe P, Travers D, Rosenau AM. Emergency Severity Index (ESI): a triage tool for emergency department care, version 4. Implementation handbook. Boston: AHRQ; 2005. [View at Publisher] [Google Scholar]
7. Farrington T, Antony J, O'Gorman KD. Continuous improvement methodologies and practices in hospitality and tourism. Int J Contemp Hosp Manag. 2018;30(1):581-600. [View at Publisher] [DOI] [Google Scholar]
8. Fazel-Asgharpour A, Barfi-dokht A, Mirhaghi AH, Shakeri MT, Kianian T. Effect of the implementation of cardiac triage scale on the time indices of patients with chest pain. Medical-Surgical Nursing Journal. 2016;5(1):e68072. [View at Publisher] [Google Scholar]
9. Tichnor-Wagner A, Wachen J, Cannata M, Cohen-Vogel L. Continuous improvement in the public school context: Understanding how educators respond to plan-do-study-act cycles. J Educ Change. 2017;18(4):465-94. [View at Publisher] [DOI] [Google Scholar]
10. Samanian A, Sadeghi T, Kazemi M. Frequency of Miss Triage Using Emergency Severity Index and Shock Index in Patients with Abdominal Trauma. Trauma Monthly. 2018;23(3):e55647. [View at Publisher] [DOI] [Google Scholar]
11. Pouyamehr A, Mirhaghi A, Eshraghi A, Sharifi MD. The effect of Heart Failure Triage Scale on used resources among heart failure patients with Dyspnea in the emergency department: a randomized clinical trial. Medical J Mashhad Univ Med Sci. 2019;61(4):1100-11. [View at Publisher] [DOI] [Google Scholar]
12. Miró Ò, Tost J, Herrero P, Jacob J, Martín-Sánchez FJ, Gil V, et al. Short-term predictive capacity of two different triage systems in patients with acute heart failure: TRICA-EAHFE study. Eur J Emerg Med. 2016;23(6):435-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Jenson A, Hansoti B, Rothman R, de Ramirez SS, Lobner K, Wallis L. Reliability and validity of emergency department triage tools in low-and middle-income countries: a systematic review. Eur J Emerg Med. 2018;25(3):154-60. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Hughes JA, Cabilan CJ, Young C, Staib A. Effect of the 4-h target on 'time-to-ECG'in patients presenting with chest pain to an emergency department: a pilot retrospective observational study. Aust Health Rev. 2018;42(2):196-202. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Ho JK, Suen LKP. Effectiveness of using the front door score to enhance the chest pain triage accuracy of emergency nurse triage decisions. J Cardiovasc Nurs. 2013;28(6):E55-64. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Frisoli TM, Nowak R, Evans KL, Harrison M, Alani M, Varghese S, et al. Henry Ford HEART score randomized trial: rapid discharge of patients evaluated for possible myocardial infarction. Circ Cardiovasc Qual Outcomes. 2017;10(10):e003617. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Abbasi N, Moghaddamnia MT, Ghanbari khaneghah A, Alizadeh R, Kazemnezhad leili E. Factors influencing the time interval from the onset of clinical symptoms to thrombolytic infusion in patients with acute myocardial infarction. Iran J Cardiovasc Nurs. 2016;4(4):48-55. [View at Publisher] [Google Scholar]
18. Mirhaghi A, Pouyamehr A, Eshraghi A, Sharifi MD. P564 Comparison between heart failure triage scale and emergency severity index to triage heart failure patients. European Heart Journal. 2018;39(suppl_1):ehy564-P564. [View at Publisher] [DOI] [Google Scholar]
19. Bohula EA, Van Diepen S, Katz J, Morrow D. Can triage to cardiac intensive care units foracute coronary sendroms be refined : data from the critical care cardiology trials network (CCCTN) registry . J Am Coll Cardiol. 2019;73(9S1):27. [View at Publisher] [DOI] [Google Scholar]
20. Gharaee R, Zohari Anboohi S, Shiri H, Nasiri M. Comparison of triage effectiveness based on ESI and HEART scale in diagnosis of outcome in patients with chest pain. J Babol Univ Med Sci. 2019;21(1):299-305. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |