Volume 20, Issue 1 (4-2023)
J Res Dev Nurs Midw 2023, 20(1): 52-55 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ajao O O, Afolalu O O, Adeniran G, Olawale S G, Agboola-Bello R. Psychosocial stress and treatment compliance among HIV/AIDS patients in a Nigerian Teaching Hospital. J Res Dev Nurs Midw 2023; 20 (1) :52-55
URL: http://nmj.goums.ac.ir/article-1-1524-en.html
URL: http://nmj.goums.ac.ir/article-1-1524-en.html
Psychosocial stress and treatment compliance among HIV/AIDS patients in a Nigerian Teaching Hospital
Olayinka Oluseyi Ajao1 

 , Olamide Olajumoke Afolalu2
, Olamide Olajumoke Afolalu2 

 , Ganiyat Adeniran3
, Ganiyat Adeniran3 

 , Stephen Gbadebo Olawale4
, Stephen Gbadebo Olawale4 

 , Rukayat Agboola-Bello3
, Rukayat Agboola-Bello3 




 , Olamide Olajumoke Afolalu2
, Olamide Olajumoke Afolalu2 

 , Ganiyat Adeniran3
, Ganiyat Adeniran3 

 , Stephen Gbadebo Olawale4
, Stephen Gbadebo Olawale4 

 , Rukayat Agboola-Bello3
, Rukayat Agboola-Bello3 


1- Medical-Surgical Nursing Unit, Department of Nursing Science, Osun State University, Nigeria
2- Mental Health Nursing Unit, Department of Nursing Science, Osun State University, Nigeria ,olamide.afolalu@uniosun.edu.ng
3- Maternal and Child Health Nursing Unit, Department of Nursing Science, Osun State University, Nigeria
4- Community Health Nursing Unit, Department of Nursing Science, Osun State University, Nigeria
2- Mental Health Nursing Unit, Department of Nursing Science, Osun State University, Nigeria ,
3- Maternal and Child Health Nursing Unit, Department of Nursing Science, Osun State University, Nigeria
4- Community Health Nursing Unit, Department of Nursing Science, Osun State University, Nigeria
Full-Text [PDF 491 kb]
(1411 Downloads)
| Abstract (HTML) (3548 Views)
Full-Text: (1040 Views)
Introduction
The Human Immunodeficiency Virus (HIV) remains a prominent global public health issue. According to the World Health Organization (WHO), approximately 33.9 - 43.8 million individuals are currently living with HIV, with nearly 40.1 million lives lost to date (1). Sub-Saharan Africa accounts for over two-thirds of the global HIV/AIDS population (2). In Nigeria, the prevalence of HIV has reached a relatively stable level, thanks to various treatment interventions implemented to improve the well-being and longevity of people living with HIV/AIDS (PLWHA) (3). Approximately 15.3 million lives have been saved as a result of Antiretroviral therapy (ART) interventions. However, despite its significant contribution to reducing the global impact of HIV infection and improving prognosis, ART adherence rates have remained relatively low (2). It is concerning that around 40% of individuals living with HIV fail to adequately adhere to their treatment, which negatively impacts their health outcomes (4).
Non-adherence to the HIV treatment regimen is frequently influenced by a combination of physical, social, and psychological factors. Xu and Munir (5) highlighted the significant impact of psychosocial factors such as stigma, discrimination, social support, substance abuse, subjective norms, and diverse cultural aspects on ART adherence and treatment compliance. These psychosocial stressors undoubtedly play a significant role in affecting adherence to ART and other treatment protocols.
Multiple studies have established a connection between HIV/AIDS treatment compliance and various psychosocial stressors. For example, an Ethiopian study involving 422 adults living with HIV reported a mental distress prevalence of 7.8%, largely attributed to social stigma and discrimination (6). These two factors frequently inflict harm upon PLWHA, instilling fear that hinders their ability to engage with others and participate in social events. Consequently, limited social interactions restrict their access to the social support necessary for optimal treatment compliance.
Numerous studies have investigated factors influencing adherence to ART worldwide, with limited research conducted within the Nigerian context. For instance, a Nigerian study examined physical and psychological factors associated with significant non-compliance to HIV/AIDS treatment, such as forgetfulness, unwillingness to adhere, avoiding clinic visits, and depression (7). However, social barriers to treatment compliance have received little attention. Considering the substantial psychosocial stress experienced by HIV patients and its impact on health outcomes, exploring psychological and social factors (both individual and environmental) that may negatively affect treatment compliance among HIV/AIDS patients can provide valuable insights. To address this research gap, this study aims to assess the relationship between psychosocial stress and treatment compliance among HIV/AIDS patients at Osun State University Teaching Hospital in Osogbo. The specific objectives are as follows: determining the stress levels of HIV/AIDS patients attending the virology clinic, identifying the primary sources of stress among the patients, assessing the level of treatment compliance, and evaluating the influence of stress on treatment compliance.
Methods
Study design and setting
For this study, a descriptive cross-sectional design was implemented at the Institute of Human Virology of Nigeria (IHVN) clinic located within Uniosun Teaching Hospital (UTH), formerly known as LAUTECH Teaching Hospital (LTH), Osogbo. The clinic operates three days a week (Monday, Tuesday, and Friday) and serves an average of 300 patients monthly. The target population consisted of HIV/AIDS patients who attended the clinic. The inclusion criteria encompassed patients who had received a diagnosis and treatment for HIV/AIDS and demonstrated a willingness to participate. Additionally, individuals above 18 years of age were included due to their increased likelihood of encountering life stressors compared to younger populations. Clients under the age of 18 and those who occasionally received treatment from other clinics were excluded from the study. Data collection involved the use of questionnaires, and information was gathered during clinic sessions over a one-month period. Prior to data collection, the approval from the ethical committee of Osun State University Teaching Hospital was presented to the attending staff nurses, and informed consent was obtained from the patients. Each patient who visited the clinic on those designated days was provided with a questionnaire to complete, which was then collected immediately upon completion.
Sample and sampling technique
Given that the study population consists of less than 10,000 individuals, a finite population correction was applied using the Taro Yamane formula. The average population of 271 HIV patients attending the Virology clinic, as obtained from the recording unit, was utilized. From this total population, a sample size of 155 was determined at a 95% confidence level. Considering a 10% non-response rate, the final sample size of 171 participants was recruited for the study using a convenient sampling technique.
Instrumentation
The data collection instrument consisted of a combination of self-structured questionnaires and standardized, validated questions adapted from existing literature. The questionnaire was divided into four sections, as outlined below.
Socio-demographic datasheet: This section collected socio-demographic information, including age, gender, ethnicity, religion, educational attainment, marital status, and occupation.
HIV/AIDS stress scale: This section included a total of 23 items, which were rated on a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). Higher scores on the scale indicated higher levels of stress. The scale, developed by Pakenham and Rinaldis (2002), was specifically designed to measure stress related to HIV/AIDS. It consisted of three subscales: social stress, instrumental stress, and emotional/existential stress, with Cronbach's alpha values of 0.85, 0.76, and 0.79, respectively (8). In this study, the overall Cronbach's alpha value for the scale was 0.91.
Sources of stress: The scale used in this study was a self-developed questionnaire consisting of eight items designed to gather information about the sources of stress among the participants. The development of the questionnaire was informed by an extensive literature review, and respondents provided "yes" or "no" responses. The scale demonstrated good internal consistency, with a Cronbach's alpha reliability coefficient of 0.81.
HIV/AIDs treatment compliance: Treatment compliance was assessed using a single-item questionnaire that was self-developed. Participants rated their level of compliance on a 7-point Likert scale, ranging from 0 (never) to 6 (always).
Reasons for noncompliance: The assessment of reasons for noncompliance to HIV treatment utilized an 18-item questionnaire developed from publicly available literature on this topic (9, 10). The questionnaire consisted of questions measured on a 4-point Likert scale, ranging from "never" (1) to "often" (4). The scale exhibited strong psychometric properties, as evidenced by a Cronbach's alpha reliability coefficient of 0.87.
The face and content validity of the questionnaire were assessed by two research experts who reviewed the questions and made necessary corrections before its utilization in the main study. The items in each questionnaire were aligned with the predetermined objectives, thoroughly scrutinized, and appropriately corrected.
Ethical consideration: Approval for the study was granted by the ethical review board of the hospital with protocol. The study obtained approval from the ethical review board of the hospital under protocol number LTH/EC/2020/11/486. Participation in the study was entirely voluntary, and participants provided their consent without any coercion. Throughout the study, the anonymity and confidentiality of the respondents were diligently maintained. The principles of beneficence and nonmaleficence were consistently upheld throughout the entire research process.
Data management
The data obtained were analyzed using SPSS version 25. Descriptive statistics were utilized to present and summarize the data. The associations between the variables of interest were examined using the chi-square test and correlation analysis.
Results
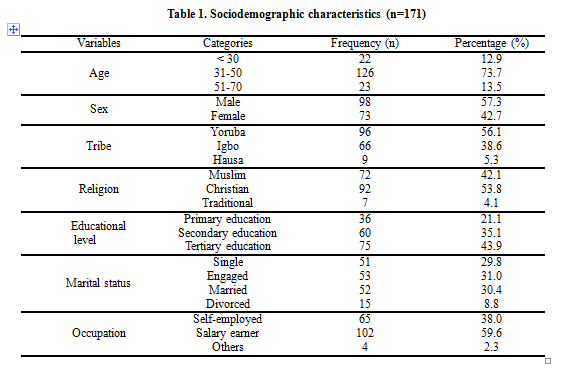
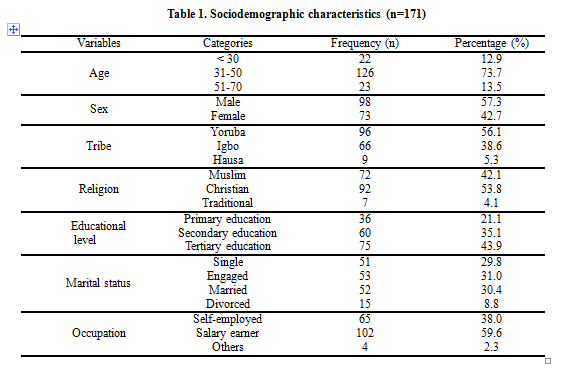
The majority of the respondents (73.7%) fell within the age range of 31-50. Among the participants, 57.3% were male, and 56.1% belonged to the Yoruba tribe. Additionally, 53.8% identified as Christians, 43.9% had attained tertiary education, and only 30.4% were married. Table 1 further reveals that 59.6% of the respondents were employed and received a salary.
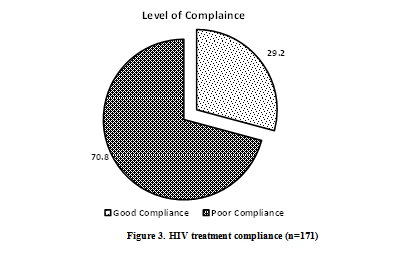
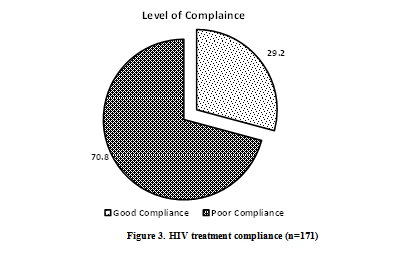
In terms of the respondents' stress levels, Figure 1 illustrates that 25.1% experienced mild stress, while a majority (61.4%) reported a moderate level of stress. Additionally, 13.5% of the respondents experienced a high level of stress. As for the sources of stress, the need for disclosure of HIV status accounted for 71.9%, followed by rejection by family and friends at 66.7%. Other significant sources of stress reported by the respondents included socioeconomic challenges (64.3%), stigma and discrimination (63.7%), and emotional problems (69.6%).
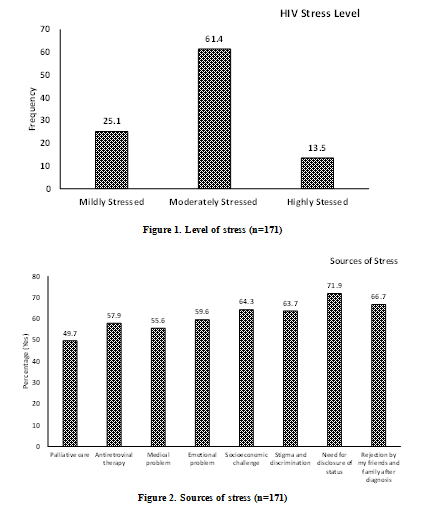
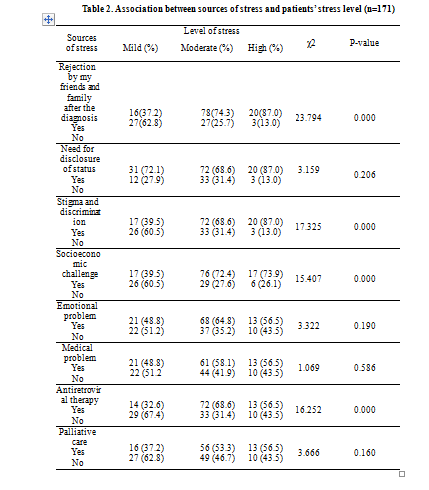
Figure 2 presents the sources of stress, while Table 2 displays the results of the chi-square test, examining the associations between the respondents' sources of stress and their stress levels. The analysis reveals several noteworthy findings. Firstly, a significant association exists between rejection by family and friends and the level of stress. Specifically, more than three-quarters of respondents who faced rejection reported experiencing a high level of stress. Similarly, among those who experienced stigma and discrimination, a larger proportion (87.0%) reported a higher level of stress, which was statistically significant. Additionally, a significant association was observed between socio-economic challenges and stress levels, with approximately three-quarters (73.9%) of respondents facing this challenge reporting a high level of stress. Moreover, more than half of the respondents (56.5%) experiencing challenges with antiretroviral therapy reported a high level of stress, which was statistically significant (p<0.005).
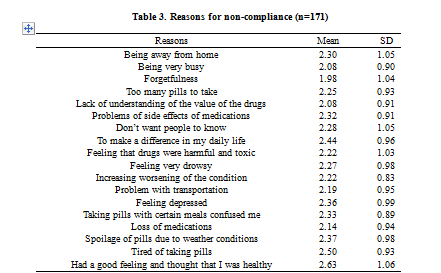
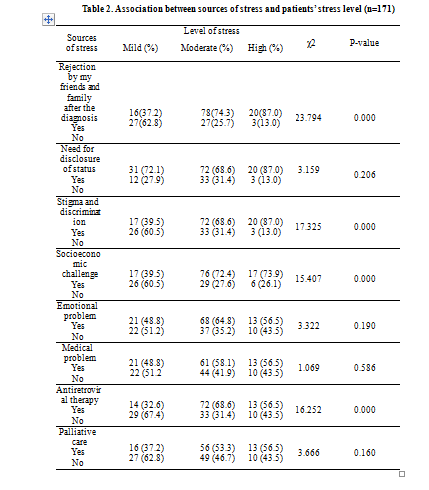
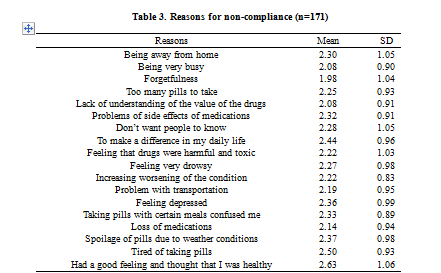
Figure 3 illustrates the treatment compliance of the respondents, indicating that 70.8% had good compliance while 29.2% had poor compliance. The reasons for noncompliance are presented in Table 3. The analysis reveals the most prominent reasons for noncompliance, which include feeling good and healthy (2.63±1.06), tired of taking pills (2.50±0.93), wanting to make a difference in daily life (2.44±0.96), spoilage of pills (2.37±0.98), and feeling depressed (2.36±0.99). On the other hand, forgetfulness was the least reported reason for noncompliance (1.98±1.04).
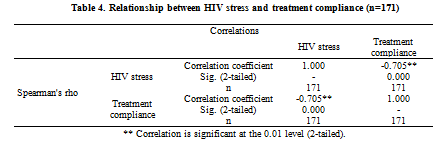
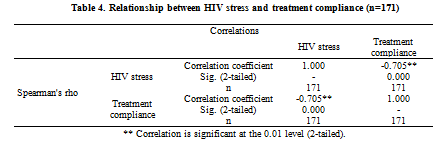
The association between psychosocial stress and treatment compliance was examined in Table 4, revealing a significant negative correlation (r = -0.705, p = 0.000). The negative sign of the correlation coefficient indicates an inverse relationship between psychosocial stress and treatment compliance. This implies that as psychosocial stress levels increase among HIV/AIDS patients, their adherence to treatment is likely to decrease. In other words, higher levels of psychosocial stress are associated with lower rates of treatment compliance.
Discussion
Data for this study was obtained from a sample of 171 HIV/AIDS patients attending the IHVN Clinic of UTH (formerly LTH). The study findings revealed that a majority of the respondents had a moderate level of stress, while a significant proportion experienced high levels of stress, suggesting a notable prevalence of psychosocial distress among these patients. These results likely stem from the multitude of stressors inherent in their life situations, combined with the challenges posed by the treatment regimen and the lack of sufficient coping mechanisms to effectively manage the psychosocial stressors associated with HIV/AIDS. Additionally, the study findings highlighted the prominent role of the need for disclosure as the most frequently reported stressor among HIV/AIDS patients. Rejection by family and friends, along with stigma and discrimination, were also identified as significant stressors experienced by the patients. These results align with previous research indicating that individuals living with HIV/AIDS often face the fear of judgment, discrimination, and isolation (11, 12). It is not surprising, given that HIV/AIDS-related stigma continues to prevail in certain areas, leading many individuals to feel uncomfortable disclosing their health status. The presence of discriminatory attitudes within certain population groups may be attributed to inadequate knowledge, misconceptions about HIV/AIDS, as well as fear of moral judgment, and anxiety (13). Furthermore, the study revealed that a significant number of the respondents identified the socio-economic issue as a major stressor, and this stressor was significantly associated with the level of stress experienced. This finding is consistent with a previous study conducted among HIV-infected individuals in South Florida, which reported that 41.1% of participants identified worsening financial status or chronic financial stress as a common stressor (14). Additionally, our findings support the research conducted by Ashaba and Kaida (15), who found that financial constraints affect the accessibility of PLWHA to HIV care, including their ability to travel to the clinic. This result is not surprising, considering the high cost of ART medications, particularly in low- and middle-income countries, which poses a significant barrier to treatment access (16). Furthermore, Chandran and Benning (17) observed that having health insurance is a determining factor for optimal healthcare utilization. Additionally, it is noteworthy that a significant relationship was found between receiving ART and stress levels, as more than half of the respondents experienced stress related to antiretroviral therapy. These factors may help explain the negative correlation between psychosocial stress and treatment adherence.
Regarding the patients’ compliance with HIV treatment, our study found that approximately three out of every ten patients reported low treatment compliance. This finding is consistent with the results of the previous study (14). However, our finding is higher compared to the study conducted by Oliveira and Caixeta (18), which reported a low adherence rate of 14%. The main reasons for non-compliance identified by the respondents were ‘having a good feeling and thought of being healthy’, ‘being tired of taking pills’, ‘feeling depressed’, and ‘wanting to make a difference in their daily lives.’ This finding is not surprising, as it is expected that patients who perceive themselves as healthy may question the necessity of taking ART. For instance, a qualitative study conducted in South Africa found that participants in their study discontinued taking medication and continued socializing with friends when they perceived an improvement in their health (19). Previous research has also reported that having to take multiple doses per day can reduce treatment compliance (20, 21), which may explain why being tired of taking pills emerged as a prominent reason for noncompliance in our study. Although some studies (22, 23) have supported the finding that depression is negatively associated with HIV treatment compliance, Chandran and Benning (17) reported contrary results, suggesting that the presence of depressive symptoms did not significantly impact treatment adherence. Many of the reasons for non-compliance identified in our study may be linked to disease progression and the subsequent steady HIV mortality rate.
Regarding the association between HIV/AIDS-related stress and treatment compliance, we found a significant positive relationship, as expected. This implies that respondents who reported higher levels of stress had more challenges with treatment compliance. These findings align with the findings of Leserman and Ironson (14), who reported that individuals experiencing three or more stressful life events were 2.5 to more than 3 times more likely to be non-compliant with HIV treatment.
The present study has certain limitations that should be considered when interpreting the findings. The generalizability of the results to a broader demographic may be limited due to the use of a single site, which may not fully represent the diversity and variability found among different locations or groups of HIV/AIDS clients. Furthermore, the exclusion of other HIV/AIDS patients in the community who were not receiving treatment at the ART clinic suggests that the entire at-risk population affected by psychosocial stress may not have been included in the study. Additionally, the use of a relatively small sample size (n=171) may restrict the generalizability of the findings.
Conclusion
This finding highlights the inverse relationship between psychosocial stress and treatment compliance, indicating that higher levels of psychosocial stress are associated with lower adherence to treatment among individuals living with HIV/AIDS. The study provides valuable insights into the complex interplay between psychosocial stress and treatment adherence within this population. These findings have important implications for healthcare professionals, policymakers, and researchers in devising strategies to alleviate the stress experienced by PLWHA. Addressing societal issues such as stigma and discrimination, ensuring equitable access to healthcare resources, and promoting mental health support services can have a positive impact on the psychosocial well-being of PLWHA and ultimately improve treatment compliance. Further research is warranted to delve deeper into these factors and unravel their underlying mechanisms.
Acknowledgement
The researchers extend their sincere gratitude to the patients who willingly participated and shared their valuable information for this study. Special appreciation is also extended to the dedicated staff of the ART clinic at UTH for their invaluable support during the data collection process. Their contribution has been instrumental in the successful completion of this research.
Funding sources
The study was self-funded by the authors.
Ethical statement
Approval for the study was obtained from the hospital's ethical review board with protocol number LTH/EC/2020/11/486.
Conflict of interest
The authors declare no conflicts of interest regarding this work and have no financial or nonfinancial relationships to disclose.
Author contributions
Study conception and design: OOA, OOA; Data collection: OOA, OOA, SOG; Data analysis and interpretation: OOA, OOA; Drafting of the article: All authors critical revision of the article: RAB, SOG, GA.
The Human Immunodeficiency Virus (HIV) remains a prominent global public health issue. According to the World Health Organization (WHO), approximately 33.9 - 43.8 million individuals are currently living with HIV, with nearly 40.1 million lives lost to date (1). Sub-Saharan Africa accounts for over two-thirds of the global HIV/AIDS population (2). In Nigeria, the prevalence of HIV has reached a relatively stable level, thanks to various treatment interventions implemented to improve the well-being and longevity of people living with HIV/AIDS (PLWHA) (3). Approximately 15.3 million lives have been saved as a result of Antiretroviral therapy (ART) interventions. However, despite its significant contribution to reducing the global impact of HIV infection and improving prognosis, ART adherence rates have remained relatively low (2). It is concerning that around 40% of individuals living with HIV fail to adequately adhere to their treatment, which negatively impacts their health outcomes (4).
Non-adherence to the HIV treatment regimen is frequently influenced by a combination of physical, social, and psychological factors. Xu and Munir (5) highlighted the significant impact of psychosocial factors such as stigma, discrimination, social support, substance abuse, subjective norms, and diverse cultural aspects on ART adherence and treatment compliance. These psychosocial stressors undoubtedly play a significant role in affecting adherence to ART and other treatment protocols.
Multiple studies have established a connection between HIV/AIDS treatment compliance and various psychosocial stressors. For example, an Ethiopian study involving 422 adults living with HIV reported a mental distress prevalence of 7.8%, largely attributed to social stigma and discrimination (6). These two factors frequently inflict harm upon PLWHA, instilling fear that hinders their ability to engage with others and participate in social events. Consequently, limited social interactions restrict their access to the social support necessary for optimal treatment compliance.
Numerous studies have investigated factors influencing adherence to ART worldwide, with limited research conducted within the Nigerian context. For instance, a Nigerian study examined physical and psychological factors associated with significant non-compliance to HIV/AIDS treatment, such as forgetfulness, unwillingness to adhere, avoiding clinic visits, and depression (7). However, social barriers to treatment compliance have received little attention. Considering the substantial psychosocial stress experienced by HIV patients and its impact on health outcomes, exploring psychological and social factors (both individual and environmental) that may negatively affect treatment compliance among HIV/AIDS patients can provide valuable insights. To address this research gap, this study aims to assess the relationship between psychosocial stress and treatment compliance among HIV/AIDS patients at Osun State University Teaching Hospital in Osogbo. The specific objectives are as follows: determining the stress levels of HIV/AIDS patients attending the virology clinic, identifying the primary sources of stress among the patients, assessing the level of treatment compliance, and evaluating the influence of stress on treatment compliance.
Methods
Study design and setting
For this study, a descriptive cross-sectional design was implemented at the Institute of Human Virology of Nigeria (IHVN) clinic located within Uniosun Teaching Hospital (UTH), formerly known as LAUTECH Teaching Hospital (LTH), Osogbo. The clinic operates three days a week (Monday, Tuesday, and Friday) and serves an average of 300 patients monthly. The target population consisted of HIV/AIDS patients who attended the clinic. The inclusion criteria encompassed patients who had received a diagnosis and treatment for HIV/AIDS and demonstrated a willingness to participate. Additionally, individuals above 18 years of age were included due to their increased likelihood of encountering life stressors compared to younger populations. Clients under the age of 18 and those who occasionally received treatment from other clinics were excluded from the study. Data collection involved the use of questionnaires, and information was gathered during clinic sessions over a one-month period. Prior to data collection, the approval from the ethical committee of Osun State University Teaching Hospital was presented to the attending staff nurses, and informed consent was obtained from the patients. Each patient who visited the clinic on those designated days was provided with a questionnaire to complete, which was then collected immediately upon completion.
Sample and sampling technique
Given that the study population consists of less than 10,000 individuals, a finite population correction was applied using the Taro Yamane formula. The average population of 271 HIV patients attending the Virology clinic, as obtained from the recording unit, was utilized. From this total population, a sample size of 155 was determined at a 95% confidence level. Considering a 10% non-response rate, the final sample size of 171 participants was recruited for the study using a convenient sampling technique.
Instrumentation
The data collection instrument consisted of a combination of self-structured questionnaires and standardized, validated questions adapted from existing literature. The questionnaire was divided into four sections, as outlined below.
Socio-demographic datasheet: This section collected socio-demographic information, including age, gender, ethnicity, religion, educational attainment, marital status, and occupation.
HIV/AIDS stress scale: This section included a total of 23 items, which were rated on a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). Higher scores on the scale indicated higher levels of stress. The scale, developed by Pakenham and Rinaldis (2002), was specifically designed to measure stress related to HIV/AIDS. It consisted of three subscales: social stress, instrumental stress, and emotional/existential stress, with Cronbach's alpha values of 0.85, 0.76, and 0.79, respectively (8). In this study, the overall Cronbach's alpha value for the scale was 0.91.
Sources of stress: The scale used in this study was a self-developed questionnaire consisting of eight items designed to gather information about the sources of stress among the participants. The development of the questionnaire was informed by an extensive literature review, and respondents provided "yes" or "no" responses. The scale demonstrated good internal consistency, with a Cronbach's alpha reliability coefficient of 0.81.
HIV/AIDs treatment compliance: Treatment compliance was assessed using a single-item questionnaire that was self-developed. Participants rated their level of compliance on a 7-point Likert scale, ranging from 0 (never) to 6 (always).
Reasons for noncompliance: The assessment of reasons for noncompliance to HIV treatment utilized an 18-item questionnaire developed from publicly available literature on this topic (9, 10). The questionnaire consisted of questions measured on a 4-point Likert scale, ranging from "never" (1) to "often" (4). The scale exhibited strong psychometric properties, as evidenced by a Cronbach's alpha reliability coefficient of 0.87.
The face and content validity of the questionnaire were assessed by two research experts who reviewed the questions and made necessary corrections before its utilization in the main study. The items in each questionnaire were aligned with the predetermined objectives, thoroughly scrutinized, and appropriately corrected.
Ethical consideration: Approval for the study was granted by the ethical review board of the hospital with protocol. The study obtained approval from the ethical review board of the hospital under protocol number LTH/EC/2020/11/486. Participation in the study was entirely voluntary, and participants provided their consent without any coercion. Throughout the study, the anonymity and confidentiality of the respondents were diligently maintained. The principles of beneficence and nonmaleficence were consistently upheld throughout the entire research process.
Data management
The data obtained were analyzed using SPSS version 25. Descriptive statistics were utilized to present and summarize the data. The associations between the variables of interest were examined using the chi-square test and correlation analysis.
Results
The majority of the respondents (73.7%) fell within the age range of 31-50. Among the participants, 57.3% were male, and 56.1% belonged to the Yoruba tribe. Additionally, 53.8% identified as Christians, 43.9% had attained tertiary education, and only 30.4% were married. Table 1 further reveals that 59.6% of the respondents were employed and received a salary.
In terms of the respondents' stress levels, Figure 1 illustrates that 25.1% experienced mild stress, while a majority (61.4%) reported a moderate level of stress. Additionally, 13.5% of the respondents experienced a high level of stress. As for the sources of stress, the need for disclosure of HIV status accounted for 71.9%, followed by rejection by family and friends at 66.7%. Other significant sources of stress reported by the respondents included socioeconomic challenges (64.3%), stigma and discrimination (63.7%), and emotional problems (69.6%).
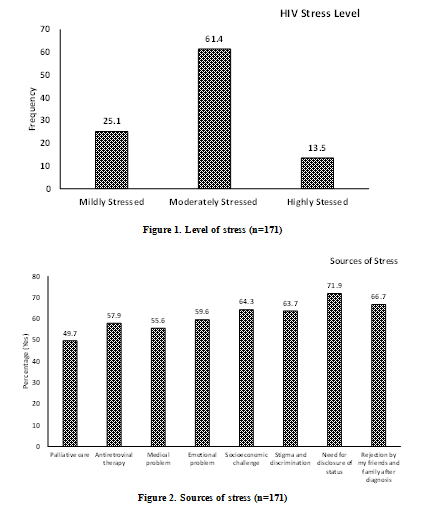
Figure 2 presents the sources of stress, while Table 2 displays the results of the chi-square test, examining the associations between the respondents' sources of stress and their stress levels. The analysis reveals several noteworthy findings. Firstly, a significant association exists between rejection by family and friends and the level of stress. Specifically, more than three-quarters of respondents who faced rejection reported experiencing a high level of stress. Similarly, among those who experienced stigma and discrimination, a larger proportion (87.0%) reported a higher level of stress, which was statistically significant. Additionally, a significant association was observed between socio-economic challenges and stress levels, with approximately three-quarters (73.9%) of respondents facing this challenge reporting a high level of stress. Moreover, more than half of the respondents (56.5%) experiencing challenges with antiretroviral therapy reported a high level of stress, which was statistically significant (p<0.005).
Figure 3 illustrates the treatment compliance of the respondents, indicating that 70.8% had good compliance while 29.2% had poor compliance. The reasons for noncompliance are presented in Table 3. The analysis reveals the most prominent reasons for noncompliance, which include feeling good and healthy (2.63±1.06), tired of taking pills (2.50±0.93), wanting to make a difference in daily life (2.44±0.96), spoilage of pills (2.37±0.98), and feeling depressed (2.36±0.99). On the other hand, forgetfulness was the least reported reason for noncompliance (1.98±1.04).
The association between psychosocial stress and treatment compliance was examined in Table 4, revealing a significant negative correlation (r = -0.705, p = 0.000). The negative sign of the correlation coefficient indicates an inverse relationship between psychosocial stress and treatment compliance. This implies that as psychosocial stress levels increase among HIV/AIDS patients, their adherence to treatment is likely to decrease. In other words, higher levels of psychosocial stress are associated with lower rates of treatment compliance.
Discussion
Data for this study was obtained from a sample of 171 HIV/AIDS patients attending the IHVN Clinic of UTH (formerly LTH). The study findings revealed that a majority of the respondents had a moderate level of stress, while a significant proportion experienced high levels of stress, suggesting a notable prevalence of psychosocial distress among these patients. These results likely stem from the multitude of stressors inherent in their life situations, combined with the challenges posed by the treatment regimen and the lack of sufficient coping mechanisms to effectively manage the psychosocial stressors associated with HIV/AIDS. Additionally, the study findings highlighted the prominent role of the need for disclosure as the most frequently reported stressor among HIV/AIDS patients. Rejection by family and friends, along with stigma and discrimination, were also identified as significant stressors experienced by the patients. These results align with previous research indicating that individuals living with HIV/AIDS often face the fear of judgment, discrimination, and isolation (11, 12). It is not surprising, given that HIV/AIDS-related stigma continues to prevail in certain areas, leading many individuals to feel uncomfortable disclosing their health status. The presence of discriminatory attitudes within certain population groups may be attributed to inadequate knowledge, misconceptions about HIV/AIDS, as well as fear of moral judgment, and anxiety (13). Furthermore, the study revealed that a significant number of the respondents identified the socio-economic issue as a major stressor, and this stressor was significantly associated with the level of stress experienced. This finding is consistent with a previous study conducted among HIV-infected individuals in South Florida, which reported that 41.1% of participants identified worsening financial status or chronic financial stress as a common stressor (14). Additionally, our findings support the research conducted by Ashaba and Kaida (15), who found that financial constraints affect the accessibility of PLWHA to HIV care, including their ability to travel to the clinic. This result is not surprising, considering the high cost of ART medications, particularly in low- and middle-income countries, which poses a significant barrier to treatment access (16). Furthermore, Chandran and Benning (17) observed that having health insurance is a determining factor for optimal healthcare utilization. Additionally, it is noteworthy that a significant relationship was found between receiving ART and stress levels, as more than half of the respondents experienced stress related to antiretroviral therapy. These factors may help explain the negative correlation between psychosocial stress and treatment adherence.
Regarding the patients’ compliance with HIV treatment, our study found that approximately three out of every ten patients reported low treatment compliance. This finding is consistent with the results of the previous study (14). However, our finding is higher compared to the study conducted by Oliveira and Caixeta (18), which reported a low adherence rate of 14%. The main reasons for non-compliance identified by the respondents were ‘having a good feeling and thought of being healthy’, ‘being tired of taking pills’, ‘feeling depressed’, and ‘wanting to make a difference in their daily lives.’ This finding is not surprising, as it is expected that patients who perceive themselves as healthy may question the necessity of taking ART. For instance, a qualitative study conducted in South Africa found that participants in their study discontinued taking medication and continued socializing with friends when they perceived an improvement in their health (19). Previous research has also reported that having to take multiple doses per day can reduce treatment compliance (20, 21), which may explain why being tired of taking pills emerged as a prominent reason for noncompliance in our study. Although some studies (22, 23) have supported the finding that depression is negatively associated with HIV treatment compliance, Chandran and Benning (17) reported contrary results, suggesting that the presence of depressive symptoms did not significantly impact treatment adherence. Many of the reasons for non-compliance identified in our study may be linked to disease progression and the subsequent steady HIV mortality rate.
Regarding the association between HIV/AIDS-related stress and treatment compliance, we found a significant positive relationship, as expected. This implies that respondents who reported higher levels of stress had more challenges with treatment compliance. These findings align with the findings of Leserman and Ironson (14), who reported that individuals experiencing three or more stressful life events were 2.5 to more than 3 times more likely to be non-compliant with HIV treatment.
The present study has certain limitations that should be considered when interpreting the findings. The generalizability of the results to a broader demographic may be limited due to the use of a single site, which may not fully represent the diversity and variability found among different locations or groups of HIV/AIDS clients. Furthermore, the exclusion of other HIV/AIDS patients in the community who were not receiving treatment at the ART clinic suggests that the entire at-risk population affected by psychosocial stress may not have been included in the study. Additionally, the use of a relatively small sample size (n=171) may restrict the generalizability of the findings.
Conclusion
This finding highlights the inverse relationship between psychosocial stress and treatment compliance, indicating that higher levels of psychosocial stress are associated with lower adherence to treatment among individuals living with HIV/AIDS. The study provides valuable insights into the complex interplay between psychosocial stress and treatment adherence within this population. These findings have important implications for healthcare professionals, policymakers, and researchers in devising strategies to alleviate the stress experienced by PLWHA. Addressing societal issues such as stigma and discrimination, ensuring equitable access to healthcare resources, and promoting mental health support services can have a positive impact on the psychosocial well-being of PLWHA and ultimately improve treatment compliance. Further research is warranted to delve deeper into these factors and unravel their underlying mechanisms.
Acknowledgement
The researchers extend their sincere gratitude to the patients who willingly participated and shared their valuable information for this study. Special appreciation is also extended to the dedicated staff of the ART clinic at UTH for their invaluable support during the data collection process. Their contribution has been instrumental in the successful completion of this research.
Funding sources
The study was self-funded by the authors.
Ethical statement
Approval for the study was obtained from the hospital's ethical review board with protocol number LTH/EC/2020/11/486.
Conflict of interest
The authors declare no conflicts of interest regarding this work and have no financial or nonfinancial relationships to disclose.
Author contributions
Study conception and design: OOA, OOA; Data collection: OOA, OOA, SOG; Data analysis and interpretation: OOA, OOA; Drafting of the article: All authors critical revision of the article: RAB, SOG, GA.
Type of study: Original Article |
Subject:
Nursing
References
1. World Health Organisation. HIV and AIDS [Fact Sheet]. World Health Organization; 2023. [Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids] [View at Publisher]
2. World Health O. HIV/AIDS [Fact sheet]. World Health Oranization; 2020. [Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids]. [View at Publisher]
3. Awofala AA, Ogundele OE. HIV epidemiology in Nigeria. Saudi Journal of biological sciences. 2018;25(4):697-703. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Spaan P, van Luenen S, Garnefski N, Kraaij V. Psychosocial interventions enhance HIV medication adherence: a systematic review and meta-analysis. Journal of health psychology. 2020;25(10-11):1326-40. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Xu L, Munir K, Kanabkaew C, Le Coeur S. Factors influencing antiretroviral treatment suboptimal adherence among perinatally HIV-infected adolescents in Thailand. PLoS One. 2017;12(2):e0172392-e. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Basha EA, Derseh BT, Haile YGE, Tafere G. Factors Affecting Psychological Distress among People Living with HIV/AIDS at Selected Hospitals of North Shewa Zone, Amhara Region, Ethiopia. AIDS Res Treat. 2019;2019:8329483. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Anyaike C, Atoyebi OA, Musa OI, Bolarinwa OA, Durowade KA, Ogundiran A, et al. Adherence to combined Antiretroviral therapy (cART) among people living with HIV/AIDS in a Tertiary Hospital in Ilorin, Nigeria. Pan Afr Med J. 2019;32:10. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Pakenham K, Rinaldis M. Development of the HIV/AIDS stress scale. Psychology and Health. 2002;17(2):203-19. [View at Publisher] [DOI] [Google scholar]
9. Hasabi IS, Shivashankarappa AB, Kachapur C, Kaulgud RS. A Study of compliance to antiretroviral therapy among HIV-infected patients at a tertiary care hospital in North Karnataka. Journal of Clinical and Diagnostic Research: JCDR. 2016;10(5):OC27. [View at Publisher] [DOI] [PMID] [Google scholar]
10. Lal V, Kant S, Dewan R, Rai SK. Reasons for non-adherence to antiretroviral therapy among adult patients receiving free treatment at a tertiary care hospital in Delhi. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine. 2010;35(1):172. [View at Publisher] [DOI] [PMID] [Google scholar]
11. Au A, Chan I, Li P, Chung R, Po LM, Yu P. Stress and health-related quality of life among HIV-infected persons in Hong Kong. AIDS and Behavior. 2004;8(2):119-29. [View at Publisher] [DOI] [PMID] [Google scholar]
12. Huang Y, Luo D, Chen X, Zhang D, Huang Z, Xiao S. HIV-Related Stress Experienced by Newly Diagnosed People Living with HIV in China: A 1-Year Longitudinal Study. International Journal of environmental research and public health. 2020;17(8):2681. [View at Publisher] [DOI] [PMID] [Google scholar]
13. Ziersch A, Walsh M, Baak M, Rowley G, Oudih E, Mwanri L. "It is not an acceptable disease": A qualitative study of HIV-related stigma and discrimination and impacts on health and wellbeing for people from ethnically diverse backgrounds in Australia. BMC Public Health. 2021;21(1):779. [View at Publisher] [DOI] [PMID] [Google scholar]
14. Leserman J, Ironson G, O'Cleirigh C, Fordiani JM, Balbin E. Stressful life events and adherence in HIV. AIDS Patient Care STDS. 2008;22(5):403-11. [View at Publisher] [DOI] [PMID] [Google scholar]
15. Ashaba S, Kaida A, Coleman JN, Burns BF, Dunkley E, O'Neil K, et al. Psychosocial challenges facing women living with HIV during the perinatal period in rural Uganda. PLoS One. 2017;12(5):e0176256. [View at Publisher] [DOI] [PMID] [Google scholar]
16. Iacob SA, Iacob DG, Jugulete G. Improving the Adherence to Antiretroviral Therapy, a Difficult but Essential Task for a Successful HIV Treatment-Clinical Points of View and Practical Considerations. Front Pharmacol. 2017;8:831. [View at Publisher] [DOI] [PMID] [Google scholar]
17. Chandran A, Benning L, Musci RJ, Wilson TE, Milam J, Adedimeji A, et al. The Longitudinal Association between Social Support on HIV Medication Adherence and Healthcare Utilization in the Women's Interagency HIV Study. AIDS and behavior. 2019;23(8):2014-24. [View at Publisher] [DOI] [PMID] [Google scholar]
18. Oliveira LdS, Caixeta LM, Martins JLR, Segati KD, Moura RS, Daher MC, et al. Adherence to antiretroviral therapy and correlation with adverse effects and coinfections in people living with HIV/AIDS in the municipality of Goiás State. Revista da Sociedade Brasileira de Medicina Tropical. 2018;51:436-44. [View at Publisher] [DOI] [PMID] [Google scholar]
19. Azia IN, Mukumbang FC, van Wyk B. Barriers to adherence to antiretroviral treatment in a regional hospital in Vredenburg, Western Cape, South Africa. Southern African Journal of HIV Medicine; Vol 17, No 1 (2016). 2016. [View at Publisher] [DOI] [PMID] [Google scholar]
20. Mizuno Y, Beer L, Huang P, Frazier EL. Factors associated with antiretroviral therapy adherence among transgender women receiving HIV medical care in the United States. LGBT health. 2017;4(3):181-7. [View at Publisher] [DOI] [PMID] [Google scholar]
21. Altice F, Evuarherhe O, Shina S, Carter G, Beaubrun A. Adherence to HIV treatment regimens: systematic literature review and meta-analysis. Patient Prefer Adherence. 2019;13:475-90. doi org/102147/PPA. 2019;35. [View at Publisher] [DOI] [PMID] [Google scholar]
22. Fonsah JY, Njamnshi AK, Kouanfack C, Qiu F, Njamnshi DM, Tagny CT, et al. Adherence to antiretroviral therapy (ART) in Yaoundé-Cameroon: association with opportunistic infections, depression, ART regimen, and side effects. PLoS One. 2017;12(1):e0170893. [View at Publisher] [DOI] [PMID] [Google scholar]
23. Wagner GJ, Ghosh-Dastidar B, Mukasa B, Linnemayr S. Changes in ART adherence relate to changes in depression as well! Evidence for the bi-directional longitudinal relationship between depression and ART adherence from a prospective study of HIV clients in Uganda. AIDS and Behavior. 2020;24:1816-24. [View at Publisher] [DOI] [PMID] [Google scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |