Volume 21, Issue 4 (12-2024)
J Res Dev Nurs Midw 2024, 21(4): 31-35 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fawzi Aldmour A, ElSayed Saleh F, Mohammad Abu Erjeh T, Premavathi S. The perception of shared governance among nurses at Dar Al Shifa Hospital in Kuwait in 2024. J Res Dev Nurs Midw 2024; 21 (4) :31-35
URL: http://nmj.goums.ac.ir/article-1-1719-en.html
URL: http://nmj.goums.ac.ir/article-1-1719-en.html
1- Dar Al Shifa Hospital, Hawally, Kuwait , dmour1988@yahoo.com
2- Dar Al Shifa Hospital, Hawally, Kuwait
2- Dar Al Shifa Hospital, Hawally, Kuwait
Full-Text [PDF 425 kb]
(775 Downloads)
| Abstract (HTML) (1807 Views)
Methods
This cross-sectional study assessed the current level of governance among nurses. Data were collected from Dar Al Shifa Hospital, which is located in Kuwait. This hospital is a 250-bed facility consisting of inpatient and outpatient departments. The target population was nurses working at Dar Al Shifa Hospital. The inclusion criteria specified that all nurses had to be currently employed at the hospital and have at least one year of experience prior to the study. Additionally, they must have at least a general nursing degree (3 years and above), a bachelor's degree, or a higher degree in nursing. Furthermore, participants must be able to read English, as the instrument is provided solely in this language. It is important to highlight that the nursing staff at Dar Al Shifa Hospital comprises a diverse range of nationalities; however, English is the official language used for communication within the hospital. In contrast, the exclusion criteria were nurses with a diploma degree (Assistant nurse, 2 years of study or less), as they are responsible for different aspects of nursing care, and any other nurses who do not meet the predetermined requirements of the inclusion criteria.
Sample size and sampling technique
Out of 819 nurses employed at the hospital, 708 were eligible to participate in the current study and met the inclusion criteria. A total of 454 participants filled out and submitted the online questionnaire, resulting in a response rate of 64.1%. The estimated sample size was calculated using the G-power software, and the result revealed that, according to a medium effect size (ES=0.25, for the analysis of variance test), the statistical power was 0.95, with a significance level of 0.05. A total of 252 participants were needed, and oversampling was targeted to account for the attrition rate. A convenience sampling method was utilized to recruit the participants, as they were selected based on their proximity and convenient accessibility for the researcher.
Measurements
Demographic data
A demographic data form was utilized for the current study. The participants were asked to indicate their gender, age, education level, years of experience in nursing, current position, current working unit, and years of experience in the current hospital. The researcher used the demographic data to determine whether the nurses' governance levels differed based on their socio-demographic information.
Index of Professional Nursing Governance (IPNG)
The IPNG scale was first developed by Robert Hess (1994) to measure nurses' perceptions of governance. In 2017, the scale was updated to a new, shorter version (IPNG 3.0), which consists of six dimensions (50 questions) representing professional governance. The IPNG is considered the most widely used instrument to measure shared governance (21). The IPNG measures the perceptions of governance of nurses on a continuum from traditional to shared and to self-governance. The IPNG measures six dimensions of governance, including: a) Nursing Personnel, which includes twelve items measuring who controls nursing personnel and related structures; b) Information, which includes nine items related to who has access to information relevant to governance activities; c) Resources, which includes nine items related to who influences resources that support professional practice; d) Participation, which includes eight items related to who creates and participates in committee structures related to governance activities at different organizational levels; e) Practice, which includes seven items measuring who controls professional practice; and f) Goals, which includes five items related to who sets goals and negotiates the resolution of conflict at different organizational levels.
In each question, participants are asked to indicate their response on a five-point Likert scale (1 = Nursing management/administration only; 2 = primarily nursing management/administration with some staff nurse input; 3 = equally shared by staff nurses and nursing management/administration; 4 = primarily staff nurses with some nursing management/administration; and 5 = staff nurses only). Scores of 1 and 2 indicate decision-making dominated by management/administration, while scores of 4 and 5 indicate more staff nurse participation in decision-making. The total scores of the IPNG determine how participants perceive the organization's governance.
IPNG 3.0 scores range from 50 to 250. Scores from 50 to 100 indicate traditional governance, where management makes decisions without staff input. Scores from 101 to 149 indicate that management has primary decision-making power, but staff input is considered. A score of 150 indicates that the decision is equally shared between staff and management. Scores of 151 to 200 indicate that staff have primary decision-making power, but management input is considered. Scores of 201 to 250 indicate self-governance, where the decision-making process is entirely based on staff input. A recent study showed that the instrument was reliable, with a Cronbach alpha of 0.91 (22). In contrast, the current study found that the Cronbach alpha for the entire IPNG tool was 0.92, indicating a high level of reliability.
Data analysis
Data were analyzed using IBM SPSS, version 27. Descriptive statistics were used to describe the participants in terms of frequencies and percentages (Gender, age, years of experience in nursing, education level, current position, current working unit, and years of experience in the current hospital). Descriptive statistics using mean and standard deviation were used to calculate the IPNG total scale and subscale scores. Analysis of variance (ANOVA) and post hoc test analysis were used to determine the differences in the perceived level of shared governance among the study participants according to their socio-demographic characteristics involving more than three groups. Moreover, the independent sample t-test was used to determine if there is a difference between participant-selected socio-demographic characteristics involving two groups (Gender, current position) and the level of perceived shared governance. The alpha level was set at ≤ 0.05 to determine the level of significance.
Data collection procedure
Following the approval of the Dar Al Shifa Institutional Review Board committee, all nurses were invited to participate in the current study, which was conducted between March 2024 and May 2024. The study's objectives, data collection methods, and the instruments used were explained to the participants. The participants were informed that their involvement in the study was entirely voluntary, and they bore no obligation to participate. The human right to anonymity and confidentiality was protected, as the nurses were not required to reveal their names. The researcher informed the participants that there were no benefits or risks associated with participating in the study. Data were collected using an online questionnaire created by the researcher through the Microsoft Forms application. The participants received a survey link via the hospital's email and were asked to complete and submit their responses. All participant responses were automatically uploaded to the researcher’s drive, from which the data were subsequently extracted. The participants were instructed to complete the questionnaire within 25 to 30 minutes.
Results
Demographic characteristics
A total of 454 nurses completed the questionnaire for this study. The majority, 424 (93.4%), were female, and 426 (93.8%) were registered nurses, with 139 (30.6%) working in closed areas. The age distribution reveals that 247 nurses (54.4%) were between 30 and 40 years old. Additionally, 284 nurses (62.6%) held a baccalaureate degree in nursing. Regarding experience, 257 nurses (56.6%) had more than 10 years in the profession, while 208 nurses (45.8%) had between 1 and 5 years of experience at Dar Al Shifa Hospital (Table 1).
Discussion
Notably, the assessment of professional nursing governance revealed that the nurses engaged in the first level of shared governance in most IPNG subscales, except for the personnel and participation subscales, which remained within the traditional range. Although the nurses perceived a shared governance level, Dar Al Shifa Hospital is still considered a new hospital implementing the shared governance model, indicating that decisions were primarily made by nursing management/administration, with some input from staff. This could be due to the hospital's recent engagement in the preparation for the Magnet journey and the ongoing implementation of shared governance models. This result is consistent with previous studies reported by (23-28), indicating that nurses perceived the organizations as shared governance environments.
The results of the access to information subscale indicated that the nurses perceived a first level of shared governance. This could be due to the existence of general nursing orientation and unit-specific orientation programs for newly hired nurses, the availability of internal hospital communication channels such as hospital email and the staff portal system, and the availability of a third-party company that provides the hospital with quarterly/annual results concerning patient and staff satisfaction. However, the nurses perceived that they had limited access to information related to compliance with the requirements of surveying agencies, strategic plans for the next few years, current nurse turnover, and vacancies available in the hospital. This could be due to the lack of involvement of frontline nurses in accreditation-related committees and teams, as well as in establishing strategic plans. Additionally, the nurses felt that they had limited access to turnover rate data, which might be attributed to the organization's nature as a private sector entity, where the turnover rate is a sensitive indicator. The result of the access to information subscale is consistent with previous studies (24,26,28-31), indicating that the nurses perceived a shared governance range in the access to information subscale.
The resources subscale results indicated that the nurses perceived the ability to control the resources that support their practices, such as daily patient assignments, regulating admission/discharge and patient transfer, obtaining supplies that support patient care, and consulting services from both within and outside the nursing department. This may be due to established policies and procedure manuals that guide and support nurses on how to complete daily nursing assignments according to patient acuity levels. Moreover, the availability of unit-based stock levels and the existence of a safety stock level policy supported the nurses in being well-equipped with all items and machines required for patient care, in addition to the formal and informal communication with the nursing department concerning supplies. Similar results have been reported in previous studies (24,26-28), indicating that nurses perceived a shared governance range in the resources subscale.
The practice subscale results indicated that the nurses perceived control over their professional practice, including policies and procedures related to patient care, determining activities of ancillary staff, educational development, selecting products used in nursing care, and determining the nursing care model in their practice. This could be due to the active role of nurses in creating and revising the policies and procedures concerning patient care, as well as the presence of a strong education department that provides continuous in-service education to nurses. These factors have empowered nurses, granting them greater authority and control over their professional practice. However, nurses reported having less control over establishing the level of qualifications for nursing positions, which could be attributed to the role of human resources in collaboration with nursing management in determining the required qualifications for these positions. Similar findings were reported (23,24,28), indicating that nurses perceived the shared governance range in the practice subscale.
The goal-setting and conflict resolution subscale results indicated that the nurses perceived having control over negotiating solutions to conflicts among nurses, between nurses and physicians, between nurses and other health services, and between nurses and nursing administration. This can be attributed to the presence of policies and procedures at Dar Al Shifa Hospital that guide the resolution of conflicts among hospital staff, monitored by the human resources department. In contrast, the nurses scored lower on negotiating solutions to conflicts between staff nurses and hospital administration. This could be because such conflicts are typically handled by the nursing administration or by a designated committee from the human resources department if the conflict is not resolved at the unit level. Similar studies have reported that nurses perceived a shared range in the goal-setting subscale (24,26,28,29).
The personnel subscale results indicated that the nurses perceived a traditional range of governance, with decisions solely controlled by the nursing administration without input from nurses. This may be attributed to the reluctance of nursing management to share power with other staff, including supervisors and head nurses, as well as the hospital's structural nature, which allows managers to make decisions concerning personnel and human resources without staff input. Multiple hospitals were surveyed, and the staff reported lower scores in the personnel subscale. For instance, a study conducted by Hess in 1988 revealed that only 1 out of 16 hospitals scored within the shared governance range (32). Recent studies have also reported that nurses perceived a traditional range in the personnel subscale (24,26-28,31).
The participation subscale results indicated that the nurses perceived a traditional range of governance, with decisions completely controlled by nursing management without input from staff nurses. This suggests that nurses have limited participation and involvement in committees concerning staffing, scheduling, and budgeting at both unit-based and department levels. In addition, they were not involved in setting the hospital-wide or unit-based mission, vision, and philosophy or in forming a wide range of committees. This could be attributed to such activities being managed at the nursing management level, with most committees attended by nursing administrative staff while nurses focus on patient care. Previous studies have reported similar findings, where nurses perceived a traditional range in the participation subscale (29,31,33).
The current study's results indicated no significant difference between the nurses and the managers in terms of governance level. This suggests that the current management position had no effect on the perceived governance level, and both nurses and managers perceived that decisions were equally shared between them. These findings are consistent with a previous study that measured nurses' perceptions of shared governance at a Jordanian University Hospital. That study indicated no statistically significant differences between staff positions and governance levels (30). Additionally, another study reported similar results (34), revealing no significant relationship between the governance and management levels.
The current study also indicated no statistically significant differences between the selected sociodemographic data of the study participants and the level of governance. This result is consistent with previous studies, which reported no statistically significant differences between the sociodemographic characteristics of the study participants and the governance level (30,34,35). However, the current study revealed statistically significant differences between years of experience at Dar Al Shifa Hospital (1<5 years, 5-10 years, and >10 years) and the level of governance (F = 3.14, P = 0.044). This finding suggests that nurses with 1<5 years of experience perceived a higher level of governance compared to those with 5-10 years and >10 years of experience. This may be because nurses with 1<5 years of experience, having recently joined the hospital, perceived an adequate level of governance as they anticipate more opportunities to engage in governance activities over time. In contrast, nurses with 5-10 years and >10 years of experience, who have already engaged extensively in governance practices, perceived a lower governance level due to practicing the same governance level for an extended period without significant development in the current governance model.
The current study was limited to Dar Al Shifa Hospital, located in Kuwait, which restricts the generalizability of the findings to other hospitals in the country. Future research should include a larger sample from diverse populations, encompassing private, Ministry of Health, and semi-governmental hospitals, and utilize bivariate and multivariate analyses to gain a more comprehensive understanding of governance perceptions among nurses on a broader scale. Additionally, the use of a self-reported questionnaire in the current study compromised the objectivity of participant responses and increased the risk of response bias.
Conclusion
In summary, this study highlights several key findings. Nurses at Dar Al Shifa Hospital perceive their engagement in decision-making at the initial level as influential in their professional practice. However, a gap was identified in their participation in committees and personnel subscales, which adhere to a traditional governance structure. No statistically significant differences were found in governance levels between staff nurses and nurse managers, nor between the selected sociodemographic data of the participants and the level of governance, except for years of experience at Dar Al Shifa Hospital. Nursing management can use the results of this study to identify the current level of governance among their nurses, establishing baseline data for future improvements.
Furthermore, based on the study's findings, the following recommendations can help achieve a higher level of governance:
- Implementation of a shared governance model in the nursing department is highly recommended to enhance staff empowerment and engagement in governance-related activities, thereby achieving a shared governance level across all IPNG subscales.
- Development of special educational programs and workshops for all nurses to enhance their knowledge and understanding of shared governance concepts
- The practice of nursing management to increase nurses' participation and engagement in designing work-related policies and procedures, decision-making, conflict resolution, staffing plans, problem-solving, and participation in committees and councils at various levels
- Encouragement of greater involvement of nurses in governance-related activities by removing any barriers that may hinder their participation. This could involve adjusting work schedules to accommodate meetings, offering additional days off for engagement in governance discussions, or designating specific days dedicated to enhancing staff involvement in decision-making processes
- Provision of nurses at all levels with special training on strategic planning, goal setting, resource management, patient flow, and material management to enhance their autonomy, empowerment, and teamwork skills
- Implementation of future research using focus groups to study nurses' governance in their specific areas; This could help identify challenges and barriers that nurses experience and potentially allow for proper interventions.
Acknowledgement
The authors express their gratitude to Dar Al Shifa Hospital and all nurses who contributed to this study.
Funding sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical statement
The study posed no actual or potential threat to the participants. However, each participant received a detailed letter outlining the key components of the study and addressing their rights, including confidentiality and the right to withdraw at any time. Additionally, the researcher obtained written approval from the authors of the Index of Professional Nursing Governance (IPNG.3), as well as written approval from the Institutional Review Board committee of Dar Al Shifa Hospital on January 16, 2024, before conducting the study.
Conflicts of interest
The authors declare that there is no conflict of interest.
Author contributions
AFA: Conceptualization and methodology, data analysis, writing the original draft, final approval. FES: Conceptualization and methodology, supervision, final approval. TMAE: Data collection, writing the original draft. SP: Data collection, critical review.
Full-Text: (304 Views)
Introduction
In today's healthcare system, a major transformation has been observed to provide collaborative, evidence-based, efficient, safe, and effective care to achieve excellence in the workplace (1). Nurses are considered the largest constituent of healthcare providers, as they play a significant role in healthcare settings; they are responsible for improving patient outcomes, ensuring transparency, and managing cultural changes (2). Building and maintaining high-quality systems in today's evolving healthcare environment can be a challenging task, especially for nurse leaders (3). Therefore, leaders have realized the importance of empowering nurses by encouraging their active participation in governance-related activities (4,5). This approach enables nurses to practice their profession with full autonomy, leading to improved patient outcomes and overall quality of care (6).
In the literature, multiple terms have been used interchangeably to describe shared governance, including shared decision-making, shared leadership, clinical governance, and collaborative governance (7). Shared governance has been defined by Omay and Buchan as "a decentralized approach which gives nurses greater authority and control over their practice and work environment; engenders a sense of responsibility and accountability; and allows active participation in the decision-making process, particularly in administrative areas from which they were excluded previously" (8). Another definition of shared governance by Hess is "a management innovation that legitimizes staff members’ decision-making control over their professional practice, while extending their influence to administrative areas previously exclusively controlled by management" (9).
The governance of professional nursing is indicated by the role of nurses in decision-making and their accountability for patient care (10). Shared governance is present when healthcare professionals, such as nurses, can exert greater influence and control over their practice (11). Nurses should involve the entire healthcare organization and all individuals, including patients, in shared governance. Models of shared governance that only involve nurses can end up being exclusionary and ultimately ineffective, as they will focus on their goals instead of the hospital as a whole (12). The primary factor that sets shared governance hospitals apart from traditional hospitals is the nurses' ability to control personnel decisions, such as hiring, transferring, promoting, and firing personnel. They can also conduct performance appraisals and disciplinary actions, oversee salaries and benefits, and create new positions within the organization (13).
The shared governance model has long been recognized as a highly effective leadership approach in the nursing profession, as it provides a supportive and empowering environment for nurses, enabling them to take greater responsibility and autonomy in regulating their work and practice (14,15). According to Porter-O’Grady, four fundamental principles of shared governance exist: partnership, accountability, equity, and ownership. These principles can be structured using the four decision-making models in healthcare institutions. The first model is unit-based governance, which derives from the nursing staff of a particular unit. The second model is councilor governance, which involves decision-making by hospital-wide nurse councils. The third model is administrative governance, in which executive leadership guides smaller nurse councils. Lastly, the congressional governance model consists of all nursing staff working together to form cabinets responsible for guiding practice (14-16).
The presence of a governance structure is important to ensure adherence to shared decision-making principles. However, a complete reliance on this structure may not help achieve the desired outcomes (17). According to Anderson, “the concept is more than a structure; the philosophy of professional accountability must be implemented” (18). Porter-O’Grady found that the complete implementation of shared governance as a philosophy and approach may require a period of 3 to 5 years (17). However, measuring the impact of shared governance is considered a challenging task because of its complex nature. It is claimed that implementing a shared governance framework can enhance the quality of care provided (4,6,14,19,20). Previous studies reported that the implementation of a shared governance framework has benefited healthcare professionals by fostering collaborative relationships between nurses, improving the quality of care for patients and clinical effectiveness, boosting staff confidence, supporting professional skills, raising professional profiles, enhancing communication between staff nurses, building on existing knowledge and skills, improving professionalism and accountability, increasing direction and focus, improving nurse retention and decreasing turnover, increasing nurse satisfaction, improving patient outcomes, and reducing duplication of effort. Such factors contribute to achieving excellence in nursing (4,6,14,19,20).
To the researcher's knowledge, no studies have been conducted in Kuwait exploring nurses' governance levels. Nurses at Dar Al Shifa Hospital play a significant role in providing high-quality care for their patients. Thus, determining their governance level and establishing baseline data can help the nursing management ensure that the nurses are moving toward excellence. This is particularly important as the nursing department is currently preparing for Magnet accreditation. The results of the current study will contribute to the existing body of research on shared governance and provide insight into how nurses perceive governance, especially in the private sector. Therefore, the objective of the current study was to assess the perception of shared governance among nurses working at Dar Al Shifa Hospital in Kuwait and to identify any differences in shared governance perception between nurses and managers, as well as differences between other sociodemographic characteristics of the study participants and their perception of shared governance. The study aimed to answer the following questions:
In today's healthcare system, a major transformation has been observed to provide collaborative, evidence-based, efficient, safe, and effective care to achieve excellence in the workplace (1). Nurses are considered the largest constituent of healthcare providers, as they play a significant role in healthcare settings; they are responsible for improving patient outcomes, ensuring transparency, and managing cultural changes (2). Building and maintaining high-quality systems in today's evolving healthcare environment can be a challenging task, especially for nurse leaders (3). Therefore, leaders have realized the importance of empowering nurses by encouraging their active participation in governance-related activities (4,5). This approach enables nurses to practice their profession with full autonomy, leading to improved patient outcomes and overall quality of care (6).
In the literature, multiple terms have been used interchangeably to describe shared governance, including shared decision-making, shared leadership, clinical governance, and collaborative governance (7). Shared governance has been defined by Omay and Buchan as "a decentralized approach which gives nurses greater authority and control over their practice and work environment; engenders a sense of responsibility and accountability; and allows active participation in the decision-making process, particularly in administrative areas from which they were excluded previously" (8). Another definition of shared governance by Hess is "a management innovation that legitimizes staff members’ decision-making control over their professional practice, while extending their influence to administrative areas previously exclusively controlled by management" (9).
The governance of professional nursing is indicated by the role of nurses in decision-making and their accountability for patient care (10). Shared governance is present when healthcare professionals, such as nurses, can exert greater influence and control over their practice (11). Nurses should involve the entire healthcare organization and all individuals, including patients, in shared governance. Models of shared governance that only involve nurses can end up being exclusionary and ultimately ineffective, as they will focus on their goals instead of the hospital as a whole (12). The primary factor that sets shared governance hospitals apart from traditional hospitals is the nurses' ability to control personnel decisions, such as hiring, transferring, promoting, and firing personnel. They can also conduct performance appraisals and disciplinary actions, oversee salaries and benefits, and create new positions within the organization (13).
The shared governance model has long been recognized as a highly effective leadership approach in the nursing profession, as it provides a supportive and empowering environment for nurses, enabling them to take greater responsibility and autonomy in regulating their work and practice (14,15). According to Porter-O’Grady, four fundamental principles of shared governance exist: partnership, accountability, equity, and ownership. These principles can be structured using the four decision-making models in healthcare institutions. The first model is unit-based governance, which derives from the nursing staff of a particular unit. The second model is councilor governance, which involves decision-making by hospital-wide nurse councils. The third model is administrative governance, in which executive leadership guides smaller nurse councils. Lastly, the congressional governance model consists of all nursing staff working together to form cabinets responsible for guiding practice (14-16).
The presence of a governance structure is important to ensure adherence to shared decision-making principles. However, a complete reliance on this structure may not help achieve the desired outcomes (17). According to Anderson, “the concept is more than a structure; the philosophy of professional accountability must be implemented” (18). Porter-O’Grady found that the complete implementation of shared governance as a philosophy and approach may require a period of 3 to 5 years (17). However, measuring the impact of shared governance is considered a challenging task because of its complex nature. It is claimed that implementing a shared governance framework can enhance the quality of care provided (4,6,14,19,20). Previous studies reported that the implementation of a shared governance framework has benefited healthcare professionals by fostering collaborative relationships between nurses, improving the quality of care for patients and clinical effectiveness, boosting staff confidence, supporting professional skills, raising professional profiles, enhancing communication between staff nurses, building on existing knowledge and skills, improving professionalism and accountability, increasing direction and focus, improving nurse retention and decreasing turnover, increasing nurse satisfaction, improving patient outcomes, and reducing duplication of effort. Such factors contribute to achieving excellence in nursing (4,6,14,19,20).
To the researcher's knowledge, no studies have been conducted in Kuwait exploring nurses' governance levels. Nurses at Dar Al Shifa Hospital play a significant role in providing high-quality care for their patients. Thus, determining their governance level and establishing baseline data can help the nursing management ensure that the nurses are moving toward excellence. This is particularly important as the nursing department is currently preparing for Magnet accreditation. The results of the current study will contribute to the existing body of research on shared governance and provide insight into how nurses perceive governance, especially in the private sector. Therefore, the objective of the current study was to assess the perception of shared governance among nurses working at Dar Al Shifa Hospital in Kuwait and to identify any differences in shared governance perception between nurses and managers, as well as differences between other sociodemographic characteristics of the study participants and their perception of shared governance. The study aimed to answer the following questions:
- What is the level of nurses' perception of shared governance?
- Is there a difference in the perceived level of shared governance between nurses and managers?
- Is there a difference in the perceived level of shared governance among nurses based on their selected socio-demographic characteristics?
Methods
This cross-sectional study assessed the current level of governance among nurses. Data were collected from Dar Al Shifa Hospital, which is located in Kuwait. This hospital is a 250-bed facility consisting of inpatient and outpatient departments. The target population was nurses working at Dar Al Shifa Hospital. The inclusion criteria specified that all nurses had to be currently employed at the hospital and have at least one year of experience prior to the study. Additionally, they must have at least a general nursing degree (3 years and above), a bachelor's degree, or a higher degree in nursing. Furthermore, participants must be able to read English, as the instrument is provided solely in this language. It is important to highlight that the nursing staff at Dar Al Shifa Hospital comprises a diverse range of nationalities; however, English is the official language used for communication within the hospital. In contrast, the exclusion criteria were nurses with a diploma degree (Assistant nurse, 2 years of study or less), as they are responsible for different aspects of nursing care, and any other nurses who do not meet the predetermined requirements of the inclusion criteria.
Sample size and sampling technique
Out of 819 nurses employed at the hospital, 708 were eligible to participate in the current study and met the inclusion criteria. A total of 454 participants filled out and submitted the online questionnaire, resulting in a response rate of 64.1%. The estimated sample size was calculated using the G-power software, and the result revealed that, according to a medium effect size (ES=0.25, for the analysis of variance test), the statistical power was 0.95, with a significance level of 0.05. A total of 252 participants were needed, and oversampling was targeted to account for the attrition rate. A convenience sampling method was utilized to recruit the participants, as they were selected based on their proximity and convenient accessibility for the researcher.
Measurements
Demographic data
A demographic data form was utilized for the current study. The participants were asked to indicate their gender, age, education level, years of experience in nursing, current position, current working unit, and years of experience in the current hospital. The researcher used the demographic data to determine whether the nurses' governance levels differed based on their socio-demographic information.
Index of Professional Nursing Governance (IPNG)
The IPNG scale was first developed by Robert Hess (1994) to measure nurses' perceptions of governance. In 2017, the scale was updated to a new, shorter version (IPNG 3.0), which consists of six dimensions (50 questions) representing professional governance. The IPNG is considered the most widely used instrument to measure shared governance (21). The IPNG measures the perceptions of governance of nurses on a continuum from traditional to shared and to self-governance. The IPNG measures six dimensions of governance, including: a) Nursing Personnel, which includes twelve items measuring who controls nursing personnel and related structures; b) Information, which includes nine items related to who has access to information relevant to governance activities; c) Resources, which includes nine items related to who influences resources that support professional practice; d) Participation, which includes eight items related to who creates and participates in committee structures related to governance activities at different organizational levels; e) Practice, which includes seven items measuring who controls professional practice; and f) Goals, which includes five items related to who sets goals and negotiates the resolution of conflict at different organizational levels.
In each question, participants are asked to indicate their response on a five-point Likert scale (1 = Nursing management/administration only; 2 = primarily nursing management/administration with some staff nurse input; 3 = equally shared by staff nurses and nursing management/administration; 4 = primarily staff nurses with some nursing management/administration; and 5 = staff nurses only). Scores of 1 and 2 indicate decision-making dominated by management/administration, while scores of 4 and 5 indicate more staff nurse participation in decision-making. The total scores of the IPNG determine how participants perceive the organization's governance.
IPNG 3.0 scores range from 50 to 250. Scores from 50 to 100 indicate traditional governance, where management makes decisions without staff input. Scores from 101 to 149 indicate that management has primary decision-making power, but staff input is considered. A score of 150 indicates that the decision is equally shared between staff and management. Scores of 151 to 200 indicate that staff have primary decision-making power, but management input is considered. Scores of 201 to 250 indicate self-governance, where the decision-making process is entirely based on staff input. A recent study showed that the instrument was reliable, with a Cronbach alpha of 0.91 (22). In contrast, the current study found that the Cronbach alpha for the entire IPNG tool was 0.92, indicating a high level of reliability.
Data analysis
Data were analyzed using IBM SPSS, version 27. Descriptive statistics were used to describe the participants in terms of frequencies and percentages (Gender, age, years of experience in nursing, education level, current position, current working unit, and years of experience in the current hospital). Descriptive statistics using mean and standard deviation were used to calculate the IPNG total scale and subscale scores. Analysis of variance (ANOVA) and post hoc test analysis were used to determine the differences in the perceived level of shared governance among the study participants according to their socio-demographic characteristics involving more than three groups. Moreover, the independent sample t-test was used to determine if there is a difference between participant-selected socio-demographic characteristics involving two groups (Gender, current position) and the level of perceived shared governance. The alpha level was set at ≤ 0.05 to determine the level of significance.
Data collection procedure
Following the approval of the Dar Al Shifa Institutional Review Board committee, all nurses were invited to participate in the current study, which was conducted between March 2024 and May 2024. The study's objectives, data collection methods, and the instruments used were explained to the participants. The participants were informed that their involvement in the study was entirely voluntary, and they bore no obligation to participate. The human right to anonymity and confidentiality was protected, as the nurses were not required to reveal their names. The researcher informed the participants that there were no benefits or risks associated with participating in the study. Data were collected using an online questionnaire created by the researcher through the Microsoft Forms application. The participants received a survey link via the hospital's email and were asked to complete and submit their responses. All participant responses were automatically uploaded to the researcher’s drive, from which the data were subsequently extracted. The participants were instructed to complete the questionnaire within 25 to 30 minutes.
Results
Demographic characteristics
A total of 454 nurses completed the questionnaire for this study. The majority, 424 (93.4%), were female, and 426 (93.8%) were registered nurses, with 139 (30.6%) working in closed areas. The age distribution reveals that 247 nurses (54.4%) were between 30 and 40 years old. Additionally, 284 nurses (62.6%) held a baccalaureate degree in nursing. Regarding experience, 257 nurses (56.6%) had more than 10 years in the profession, while 208 nurses (45.8%) had between 1 and 5 years of experience at Dar Al Shifa Hospital (Table 1).
IPNG total score and subscales scores
The results of the current study indicated that the overall IPNG mean score was 100.3, falling under the first level of the shared governance range [101-149]. Likewise, all subscales of the IPNG remained within the shared governance range, except for the participation and personnel subscales, which were within the traditional governance range (Table 2). In accessing information (i.e., who has access to information related to governance activities), the nurses' mean score was 18.9, falling at the border of the shared governance range [19-36]. Regarding the practice subscale (i.e., who controls professional practice), the nurses' mean score was 16.1, falling under the shared governance range [15-28]. In the goal-setting subscale (i.e., who has the ability to set goals and negotiate the resolution of conflicts), the nurses' mean score was 10.3, falling under the shared governance range [10-20]. Finally, in the resource subscale (i.e., who controls the resources that support professional practice), the nurses' mean score was 21.9, which was under the shared governance range [19-36].
The results of the current study indicated that the overall IPNG mean score was 100.3, falling under the first level of the shared governance range [101-149]. Likewise, all subscales of the IPNG remained within the shared governance range, except for the participation and personnel subscales, which were within the traditional governance range (Table 2). In accessing information (i.e., who has access to information related to governance activities), the nurses' mean score was 18.9, falling at the border of the shared governance range [19-36]. Regarding the practice subscale (i.e., who controls professional practice), the nurses' mean score was 16.1, falling under the shared governance range [15-28]. In the goal-setting subscale (i.e., who has the ability to set goals and negotiate the resolution of conflicts), the nurses' mean score was 10.3, falling under the shared governance range [10-20]. Finally, in the resource subscale (i.e., who controls the resources that support professional practice), the nurses' mean score was 21.9, which was under the shared governance range [19-36].
Table 2. Descriptive statistics for the total index of professional nursing governance (IPNG) and subscales scores (n=454).PNG) |
An independent samples t-test was conducted to determine whether there was a difference in shared governance scores between staff nurses and nurse managers. Levene's test was performed to verify the test's assumptions, and the result revealed a p-value of 0.470. This indicates that the assumption of equal variance was not violated. For the differences between the two group scores, the result showed that there was no statistically significant difference in the shared governance scores (F = 0.524, P = 0.231). A one-way ANOVA with a post hoc test was used to assess if there were differences in the participants' shared governance scores and selected sociodemographic data (Age, education level, working unit, and years of experience in the nursing profession). Levene's test revealed a p-value of 0.199, indicating that the homogeneity of variance assumption was not violated. The analysis of ANOVA showed no significant difference between the participants' governance levels and their selected sociodemographic data. The years of experience at Dar Al Shifa Hospital was the only sociodemographic variable that showed a statistically significant difference with the shared governance level (F = 3.14, P = 0.044) (Table 3).
Table 3. Index of Professional Nursing Governance total score by years of experience in Dar Al Shifa Hospital, One-Way ANOVA.PNG) |
A post hoc analysis using the least significant difference test was conducted. The results indicated a statistically significant difference between participants with 1 to 5 years of experience and those with 5 to 10 years of experience (P = 0.036). Additionally, there was a significant difference between staff with 1 to 5 years of experience and those with more than 10 years of experience (P = 0.043) (Table 4).
Table 4. Multiple comparisons between the years of experience in Dar Al Shifa Hospital, Post Hoc test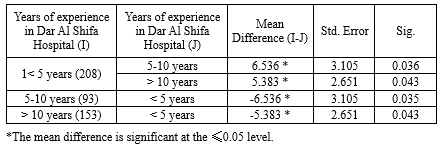 |
Discussion
Notably, the assessment of professional nursing governance revealed that the nurses engaged in the first level of shared governance in most IPNG subscales, except for the personnel and participation subscales, which remained within the traditional range. Although the nurses perceived a shared governance level, Dar Al Shifa Hospital is still considered a new hospital implementing the shared governance model, indicating that decisions were primarily made by nursing management/administration, with some input from staff. This could be due to the hospital's recent engagement in the preparation for the Magnet journey and the ongoing implementation of shared governance models. This result is consistent with previous studies reported by (23-28), indicating that nurses perceived the organizations as shared governance environments.
The results of the access to information subscale indicated that the nurses perceived a first level of shared governance. This could be due to the existence of general nursing orientation and unit-specific orientation programs for newly hired nurses, the availability of internal hospital communication channels such as hospital email and the staff portal system, and the availability of a third-party company that provides the hospital with quarterly/annual results concerning patient and staff satisfaction. However, the nurses perceived that they had limited access to information related to compliance with the requirements of surveying agencies, strategic plans for the next few years, current nurse turnover, and vacancies available in the hospital. This could be due to the lack of involvement of frontline nurses in accreditation-related committees and teams, as well as in establishing strategic plans. Additionally, the nurses felt that they had limited access to turnover rate data, which might be attributed to the organization's nature as a private sector entity, where the turnover rate is a sensitive indicator. The result of the access to information subscale is consistent with previous studies (24,26,28-31), indicating that the nurses perceived a shared governance range in the access to information subscale.
The resources subscale results indicated that the nurses perceived the ability to control the resources that support their practices, such as daily patient assignments, regulating admission/discharge and patient transfer, obtaining supplies that support patient care, and consulting services from both within and outside the nursing department. This may be due to established policies and procedure manuals that guide and support nurses on how to complete daily nursing assignments according to patient acuity levels. Moreover, the availability of unit-based stock levels and the existence of a safety stock level policy supported the nurses in being well-equipped with all items and machines required for patient care, in addition to the formal and informal communication with the nursing department concerning supplies. Similar results have been reported in previous studies (24,26-28), indicating that nurses perceived a shared governance range in the resources subscale.
The practice subscale results indicated that the nurses perceived control over their professional practice, including policies and procedures related to patient care, determining activities of ancillary staff, educational development, selecting products used in nursing care, and determining the nursing care model in their practice. This could be due to the active role of nurses in creating and revising the policies and procedures concerning patient care, as well as the presence of a strong education department that provides continuous in-service education to nurses. These factors have empowered nurses, granting them greater authority and control over their professional practice. However, nurses reported having less control over establishing the level of qualifications for nursing positions, which could be attributed to the role of human resources in collaboration with nursing management in determining the required qualifications for these positions. Similar findings were reported (23,24,28), indicating that nurses perceived the shared governance range in the practice subscale.
The goal-setting and conflict resolution subscale results indicated that the nurses perceived having control over negotiating solutions to conflicts among nurses, between nurses and physicians, between nurses and other health services, and between nurses and nursing administration. This can be attributed to the presence of policies and procedures at Dar Al Shifa Hospital that guide the resolution of conflicts among hospital staff, monitored by the human resources department. In contrast, the nurses scored lower on negotiating solutions to conflicts between staff nurses and hospital administration. This could be because such conflicts are typically handled by the nursing administration or by a designated committee from the human resources department if the conflict is not resolved at the unit level. Similar studies have reported that nurses perceived a shared range in the goal-setting subscale (24,26,28,29).
The personnel subscale results indicated that the nurses perceived a traditional range of governance, with decisions solely controlled by the nursing administration without input from nurses. This may be attributed to the reluctance of nursing management to share power with other staff, including supervisors and head nurses, as well as the hospital's structural nature, which allows managers to make decisions concerning personnel and human resources without staff input. Multiple hospitals were surveyed, and the staff reported lower scores in the personnel subscale. For instance, a study conducted by Hess in 1988 revealed that only 1 out of 16 hospitals scored within the shared governance range (32). Recent studies have also reported that nurses perceived a traditional range in the personnel subscale (24,26-28,31).
The participation subscale results indicated that the nurses perceived a traditional range of governance, with decisions completely controlled by nursing management without input from staff nurses. This suggests that nurses have limited participation and involvement in committees concerning staffing, scheduling, and budgeting at both unit-based and department levels. In addition, they were not involved in setting the hospital-wide or unit-based mission, vision, and philosophy or in forming a wide range of committees. This could be attributed to such activities being managed at the nursing management level, with most committees attended by nursing administrative staff while nurses focus on patient care. Previous studies have reported similar findings, where nurses perceived a traditional range in the participation subscale (29,31,33).
The current study's results indicated no significant difference between the nurses and the managers in terms of governance level. This suggests that the current management position had no effect on the perceived governance level, and both nurses and managers perceived that decisions were equally shared between them. These findings are consistent with a previous study that measured nurses' perceptions of shared governance at a Jordanian University Hospital. That study indicated no statistically significant differences between staff positions and governance levels (30). Additionally, another study reported similar results (34), revealing no significant relationship between the governance and management levels.
The current study also indicated no statistically significant differences between the selected sociodemographic data of the study participants and the level of governance. This result is consistent with previous studies, which reported no statistically significant differences between the sociodemographic characteristics of the study participants and the governance level (30,34,35). However, the current study revealed statistically significant differences between years of experience at Dar Al Shifa Hospital (1<5 years, 5-10 years, and >10 years) and the level of governance (F = 3.14, P = 0.044). This finding suggests that nurses with 1<5 years of experience perceived a higher level of governance compared to those with 5-10 years and >10 years of experience. This may be because nurses with 1<5 years of experience, having recently joined the hospital, perceived an adequate level of governance as they anticipate more opportunities to engage in governance activities over time. In contrast, nurses with 5-10 years and >10 years of experience, who have already engaged extensively in governance practices, perceived a lower governance level due to practicing the same governance level for an extended period without significant development in the current governance model.
The current study was limited to Dar Al Shifa Hospital, located in Kuwait, which restricts the generalizability of the findings to other hospitals in the country. Future research should include a larger sample from diverse populations, encompassing private, Ministry of Health, and semi-governmental hospitals, and utilize bivariate and multivariate analyses to gain a more comprehensive understanding of governance perceptions among nurses on a broader scale. Additionally, the use of a self-reported questionnaire in the current study compromised the objectivity of participant responses and increased the risk of response bias.
Conclusion
In summary, this study highlights several key findings. Nurses at Dar Al Shifa Hospital perceive their engagement in decision-making at the initial level as influential in their professional practice. However, a gap was identified in their participation in committees and personnel subscales, which adhere to a traditional governance structure. No statistically significant differences were found in governance levels between staff nurses and nurse managers, nor between the selected sociodemographic data of the participants and the level of governance, except for years of experience at Dar Al Shifa Hospital. Nursing management can use the results of this study to identify the current level of governance among their nurses, establishing baseline data for future improvements.
Furthermore, based on the study's findings, the following recommendations can help achieve a higher level of governance:
- Implementation of a shared governance model in the nursing department is highly recommended to enhance staff empowerment and engagement in governance-related activities, thereby achieving a shared governance level across all IPNG subscales.
- Development of special educational programs and workshops for all nurses to enhance their knowledge and understanding of shared governance concepts
- The practice of nursing management to increase nurses' participation and engagement in designing work-related policies and procedures, decision-making, conflict resolution, staffing plans, problem-solving, and participation in committees and councils at various levels
- Encouragement of greater involvement of nurses in governance-related activities by removing any barriers that may hinder their participation. This could involve adjusting work schedules to accommodate meetings, offering additional days off for engagement in governance discussions, or designating specific days dedicated to enhancing staff involvement in decision-making processes
- Provision of nurses at all levels with special training on strategic planning, goal setting, resource management, patient flow, and material management to enhance their autonomy, empowerment, and teamwork skills
- Implementation of future research using focus groups to study nurses' governance in their specific areas; This could help identify challenges and barriers that nurses experience and potentially allow for proper interventions.
Acknowledgement
The authors express their gratitude to Dar Al Shifa Hospital and all nurses who contributed to this study.
Funding sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical statement
The study posed no actual or potential threat to the participants. However, each participant received a detailed letter outlining the key components of the study and addressing their rights, including confidentiality and the right to withdraw at any time. Additionally, the researcher obtained written approval from the authors of the Index of Professional Nursing Governance (IPNG.3), as well as written approval from the Institutional Review Board committee of Dar Al Shifa Hospital on January 16, 2024, before conducting the study.
Conflicts of interest
The authors declare that there is no conflict of interest.
Author contributions
AFA: Conceptualization and methodology, data analysis, writing the original draft, final approval. FES: Conceptualization and methodology, supervision, final approval. TMAE: Data collection, writing the original draft. SP: Data collection, critical review.
Type of study: Original Article |
Subject:
Nursing
References
1. Salmond SW, Echevarria M. Healthcare Transformation and Changing Roles for Nursing. Orthop Nurs. 2017;36(1):12-25. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Gerard S, Owens D, Oliver P. Nurses' perception of shared decision-making processes. J Nurs Adm. 2016;46(9):477-83. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Dearmon VA, Riley BH, Mestas LG, Buckner EB. Bridge to shared governance: developing leadership of frontline nurses. Nurs Adm Q. 2015;39(1):69-77. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Barden AM, Griffin MTQ, Donahue M, Fitzpatrick JJ. Shared governance and empowerment in registered nurses working in a hospital setting. Nurs Adm Q. 2011;35(3):212-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Wilson EM. Evaluating Shared Governance For Nursing Excellence. UNLV Theses, Dissertations, Professional Papers, and Capstones. 2013. [View at Publisher] [DOI] [Google Scholar]
6. Cohen CS. Leveraging the power of shared governance. Walden Dissertations and Doctoral Studies. 2015. [View at Publisher] [Google Scholar]
7. Jordan J. Perceptions of shared governance and structural empowerment among nurses working in magnet hospitals. Widener University ProQuest Dissertations & Theses. 2019. [View at Publisher] [Google Scholar]
8. O'May F, Buchan J. Shared governance: A literature review. Int J Nurs Stud. 1999;36(4):281-300. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Hess, R. The measurement of professional governance: Scoring guidelines and benchmarks. Hobe Sound, FL:Forum for Shared Governance;2017. [View at Publisher]
10. Porter-O'Grady T, Clavelle JT. The Structural Framework for Nursing Professional Governance:: Foundation for Empowerment. Nurs Lead. 2020;18(2):181-9. [View at Publisher] [DOI] [Google Scholar]
11. Robertson-Malt S, Chapman Y. Finding the right direction: the importance of open communication in a governance model of nurse management. Contemp Nurse. 2008;29(1):60-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Fawzia F, Mohammed S. Perception of Shared Governance and Its Relation to Nurses Empowerment in Benha and Menoufia University Hospitals. 2015. [View at Publisher]
13. Hess RG. From bedside to boardroom - Nursing shared governance. Online J Issues Nurs. 2004;9(1):5-16. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Alrwaihi S, Kehyayan V, Johnson JM. Interdisciplinary shared governance: A literature review. J Nurs Educ Pract. 2018;8(4):43. [View at Publisher] [DOI] [Google Scholar]
15. Porter-O'Grady T. Is shared governance still relevant? J Nurs Adm. 2001;31(10):468-73. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Overcash J, Petty LJ, Brown S. Perceptions of shared governance among nurses at a midwestern hospital. Nurs Adm Q. 2012;36(4):E1-11. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. O'Grady TP, Clavelle JT. Transforming Shared Governance: Toward Professional Governance for Nursing. J Nurs Adm. 2021;51(4):206-11. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Anderson EF. A case for measuring governance. Nurs Adm Q. 2011;35(3):197-203. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Kutney-Lee A, Germack H, Hatfield L, Kelly S, Maguire P, Dierkes A, et al. Nurse Engagement in Shared Governance and Patient and Nurse Outcomes. J Nurs Adm. 2016;46(11):605-12. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Torres A, Kunishige N, Morimoto D, Hanzawa T, Ebesu M, Fernandez J, et al. Shared governance: a way to improve the care in an inpatient rehabilitation facility. Rehabil Nurs. 2015;40(2):69-73. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Kyytsönen M, Tomietto M, Huhtakangas M, Kanste O. Research on hospital-based shared governance: a scoping review.Int J Health Gov. 2020;25(4):371-86. [View at Publisher] [DOI] [Google Scholar]
28. Abd El Gwad Maged YHAF, Bassiouni NA, Ghanem Atalla AD. Relationship between Nursing Governance and Shared Leadership Style as Perceived by Nurses. International Journal of Novel Research in Healthcare and Nursing. 2021;8(2):34-49. [View at Publisher] [Google Scholar]
29. Abou Hashish EA, Fargally SM. Assessment of professional nursing governance and hospital magnet components at Alexandria Medical Research Institute, Egypt. J Nurs Educ Pract. 2018;8(3):37. [View at Publisher] [DOI] [Google Scholar]
30. Khraisat O, Al-awamreh K, Hamdan M, AL-Bashtawy M, khawaldeh A Al, Alqudah M, et al. Shared governance: a children's hospital journey to clinical nursing excellence. J Res Nurs. 2020;25(4):347-58. [View at Publisher] [DOI] [PMID] [Google Scholar]
31. Atalla ADG, Sharif LS, Katooa NE, Kandil FS, Mahsoon A, Mahmoud Elseesy NA. Relationship between nurses' perception of professional shared governance and their career motivation: A cross-sectional study. Int J Nurs Sci. 2023;10(4):485-91. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Al-Hamdan Z, Abu- Erjeh T, Bawadi H, Ahmad M, Alhamdan M, Khalili H. Shared Governance among Nurses: A Descriptive Study from Jordan. Jordan Journal of Nursing Research. 2022;1(2):47-54. [View at Publisher] [DOI] [Google Scholar]
33. Speroni KG, Budhathoki C, Walters C, Dutton S, Mackay P, Oguariri RM. Survey Research: Do All RN Types Have the Same Perceptions Regarding Professional Nursing Governance? J Nurs Adm. 2022;52(5):258-65. [View at Publisher] [DOI] [PMID] [Google Scholar]
34. Aljohani EH, Hamouda GM, Banakhar MA. Nurses' Perception toward Shared Governance in Clinical Practice at General Hospitals in Jeddah City. Evidence-Based Nursing Research. 2020;2(3):11. [View at Publisher] [DOI] [Google Scholar]
35. Ahmed A, El -Sayed K, EL Demerdash S. Registered Nurses' Perception Regarding Shared Governance and Its Relation to their Job Satisfaction. Tanta Scientific Nursing Journal. 2023;29(2):255-71. [View at Publisher] [DOI] [Google Scholar]
36. Al-Faouri I, Bany M, Abdullah K. Perception of Shared Governance among Registered Nurses in a Jordanian University Hospital. 2014;4(6):254-62. [View at Publisher] [Google Scholar]
37. Kaddourah B, Al-Tannir M, Kakish S, AlFayyad I. Perception of Shared Governance Among Registered Nurses in Ambulatory Care Center at a Tertiary Care Hospital in Saudi Arabia. Cureus. 2020;12(6):e8736. [View at Publisher] [DOI] [PMID] [Google Scholar]
39. Weaver SH, Hess RG, Williams B, Guinta L, Paliwal M. Measuring shared governance: One healthcare system's experience. Nurs Manage. 2018;49(10):11-4. [View at Publisher] [DOI] [PMID] [Google Scholar]
40. Sayed S, Ahmed M, Bakr M, Sherief NM. Assessment of Professional Nursing Governance among Egyptian Nurses. Menoufia Nursing Journal. 2019;4(2):23-9. [View at Publisher] [DOI] [Google Scholar]
42. Howell JN, Frederick J, Olinger B, Leftridge D, Bell T, Hess R, et al. Can nurses govern in a government agency? J Nurs Adm. 2001;31(4):187-95. [View at Publisher] [DOI] [PMID] [Google Scholar]
43. George VM, Burke LJ, Rodgers BL. Research-based planning for change: assessing nurses' attitudes toward governance and professional practice autonomy after hospital acquisition. J Nurs Adm. 1997;27(5):53-61. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





.PNG)
