Volume 22, Issue 1 (3-2025)
J Res Dev Nurs Midw 2025, 22(1): 25-31 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Afolalu O O, Adebiyi P A, Akpor O A, Adesina K A, Makinde S O, Olawale S G, et al . Nurses' perspectives on the challenges of sickle cell disease management and associated factors in a teaching hospital in south-western Nigeria. J Res Dev Nurs Midw 2025; 22 (1) :25-31
URL: http://nmj.goums.ac.ir/article-1-1918-en.html
URL: http://nmj.goums.ac.ir/article-1-1918-en.html
Olamide O Afolalu1 

 , Peter A Adebiyi2
, Peter A Adebiyi2 

 , Oluwaseyi A Akpor2
, Oluwaseyi A Akpor2 

 , Kamoru A Adesina2
, Kamoru A Adesina2 

 , Scholastica O Makinde2
, Scholastica O Makinde2 

 , Stephen G Olawale2
, Stephen G Olawale2 

 , Juliet I. Adegoke2
, Juliet I. Adegoke2 

 , Temitope F Adekomi2
, Temitope F Adekomi2 

 , Roseline O Folami2
, Roseline O Folami2 




 , Peter A Adebiyi2
, Peter A Adebiyi2 

 , Oluwaseyi A Akpor2
, Oluwaseyi A Akpor2 

 , Kamoru A Adesina2
, Kamoru A Adesina2 

 , Scholastica O Makinde2
, Scholastica O Makinde2 

 , Stephen G Olawale2
, Stephen G Olawale2 

 , Juliet I. Adegoke2
, Juliet I. Adegoke2 

 , Temitope F Adekomi2
, Temitope F Adekomi2 

 , Roseline O Folami2
, Roseline O Folami2 


1- Department of Medical-Surgical Nursing, College of Health Sciences, Faculty of Nursing Sciences, Osun State University, Osogbo, Osun State Nigeria , olamide.afolalu@uniosun.edu.ng
2- Department of Medical-Surgical Nursing, College of Health Sciences, Faculty of Nursing Sciences, Osun State University, Osogbo, Osun State Nigeria
2- Department of Medical-Surgical Nursing, College of Health Sciences, Faculty of Nursing Sciences, Osun State University, Osogbo, Osun State Nigeria
Full-Text [PDF 551 kb]
(531 Downloads)
| Abstract (HTML) (1588 Views)
Discussion
The findings of this study provide important insight into the several multifactorial challenges faced by nurses in the management of patients with SCD in a Nigerian hospital setting. Nurses in this study reported a variety of obstacles that are mostly patients and systems-related, including behavior and non-compliance to treatment, opioid addiction in pain management, sickle cell unit congestion and overcrowding, drug-seeking behaviors, and patient-staff disputes. Some of the difficulties the research participants faced are comparable to those that have been previously reported in published evidence-based scholarly articles (21-23). In the context of SCD management, understanding nurses' demographic characteristics is crucial to gaining adequate insight into how they address the challenges associated with this ailment. Most of the respondents in this study fall within the age range of 31-40 years with a mean age of 24.3 years. This age distribution affirms that the hospital's staff is comparatively young, which could affect their training and expertise in treating chronic illnesses like SCD. A younger workforce might be more up-to-date on the latest developments in healthcare procedures, but they might also lack the knowledge and experience necessary to handle complicated medical situations, such as long-term SCD management that necessitates multidisciplinary collaboration (22).
The most significant challenges considered to be associated with patients' negative behaviors as identified by the respondents were those relating to failure to comply with medical advice, with 73.1% of respondents reporting this as an issue, and 80.9% pointing to addiction of patients with SCD to opioids and other analgesics. Non-compliance in chronic conditions such as SCD can arise from various factors, including a lack of understanding of the disease and its severity, the chronic nature of the illness, or psychological factors such as worry or fear of treatment (22). The results of this study are consistent with another Nigerian study (24) that found non-adherence to therapy as a common occurrence among patients with SCD, frequently brought on by misunderstandings about the illness or the adverse effects of drugs. Poorer health outcomes, worsening symptoms, and maybe more frequent hospitalizations can result from patient non-compliance. Noteworthy, a crucial component of therapy for people with SCD is alleviating pain, especially during sickle cell crises. However, the risk of opiate addiction makes it more difficult to manage pain in these people. Nurses in our study expressed concerns that some patients often misuse pain medications, evidenced by some of the patients' ringing bells for nurses’ attention, to request additional pain medications before the next due dose. This mostly complicates treatment regimens, making treatment plans more difficult. Some researchers support this issue by highlighting the difficulties in controlling pain in patients with SCD while also addressing opioid dependence concerns (25,26). Opioid abuse can make it difficult to strike the right balance between pain management and dependency risk; thereby necessitating careful and more sophisticated nursing intervention.
Overcrowding and patient-staff conflicts were also mentioned by our participants as major challenges, with 58.6% and 68.9% of them citing them as such, respectively. This issue is prevalent in many low-resource hospitals where a high volume of patients, limited bed spaces, and insufficient personnel put an additional burden on medical professionals. This problem could have been aggravated by a lack of specialized clinics, specifically built for the care of patients with SCD (27). A previous study shows that in Nigeria's emergency tertiary hospitals, overcrowding and bed shortages have been serious health problems for over a decade (28). Overcrowding increases the rates of nurse turnover, resulting in lower quality of care because nurses are frequently overworked and unable to give individualized care, which is especially important for managing chronic conditions such as patients with SCD who need close observation (29). The patients' discontent with care or displeasure with how their pain is managed may be the cause of the conflicts our study found. Consistent with the findings of other studies, disagreements between patients and medical professionals might cause a communication breakdown, which can affect the nurse-patient relationship (25,30). The ability to provide appropriate treatment may be further hampered by this strain since managing chronic disorders like SCD requires cooperation and confidence.
The findings of this study also showed the factors associated with the challenges experienced by nurses. The most common obstacle, as reported by 90.2% of the participants, was insufficient funds to begin therapy. This aligns with the results of earlier studies that have identified financial limitations as the primary barrier to providing quality healthcare in environments with few resources, such as Nigeria (22,24). Insufficient funds negatively impact patients’ ability to receive blood transfusions, necessary drugs such as opioids, and other supportive therapies needed to control SCD symptoms (21,26). This financial strain may result in inadequate or postponed treatment, which would impair patient outcomes and raise the system's and families' overall healthcare costs.
Furthermore, over 80% of our respondents identified inadequate follow-up care as another significant factor associated with the challenges of managing patients with SCD. Intermittent trips to healthcare professionals and inadequate monitoring of patient's health status are common issues in managing chronic conditions like SCD. However, this could be exacerbated by financial constraints that limit patients' adherence to the usage of health facilities (24). Also, worthy of note is the 63.3% of respondents who acknowledged a lack of proper history taking as the least common challenge. This number emphasizes a crucial component of patient care even though it is lower than the other factors. Adequate history-taking is fundamental for accurate diagnosis, treatment planning, and monitoring of disease progression (31). Incomplete or improper pre-consultation history taking can result in mismanagement, delayed diagnoses, and unnecessary complications (32). This implies that while taking a patient's history may not present as much of a problem as financial considerations, it is still a crucial component of care that cannot be disregarded. Improving patients’ education, expanding access to affordable healthcare, and incorporating sociocultural factors into treatment regimens should be the main goals of initiatives to address these issues. Therefore, the findings of this study support the necessity for a comprehensive strategy in tackling the difficulties of managing chronic conditions like SCD and are in line with the larger body of literature.
While this study assessed the challenges experienced by nurses in managing patients with SCD, utilization of a single site setting in Southwest Nigeria, which does not allow for comparison between two or more settings was a study limitation. This could compromise external validity by making it challenging to extrapolate results to different contexts where problems might be different. Future studies could include responses from diverse settings, with a mix of different professionals’ perspectives. Additionally, responses involving self-reports, such as surveys, entail having knowledge and memory of information, which presents a potential for both social desirability and recall biases. There is a plausible hypothesis that some of the nurses might exaggerate or underestimate the challenges faced during SCD management. Notwithstanding the drawbacks, this study may serve as a basis for subsequent initiatives that seek to improve health outcomes and support for patients with SCD.
Conclusion
This study highlights the significant challenges faced by nurses in a Nigerian hospital when caring for patients with SCD, including systemic and patient-related barriers. Key issues such as unit congestion, opioid addiction, patient non-compliance, and resource shortages complicate care delivery. Financial constraints are particularly pressing, hindering access to essential medications and treatments, while overcrowding and inadequate follow-up care further strain the healthcare system. To improve patients’ outcomes in low-resource settings like Nigeria, it is crucial to enhance training for nurses and patients to better understand the disease and treatment regimens. Improving healthcare infrastructure and ensuring the availability of necessary resources will also facilitate effective care delivery. Prioritizing the alleviation of financial constraints is essential for effective SCD treatment. Continuous educational training for patients can help reduce opioid addiction and promote adherence to treatment. Additionally, targeted training programs for nurses can address systemic issues, ultimately leading to improved patient care and health outcomes.
Acknowledgement
The research team appreciates the valuable contribution of the nurses for their time in participating in this study.
Funding sources
None declared.
Ethical statement
Written permission was obtained from the hospital where the nurses were recruited, with protocol number UTH/EC/2022/10/657. The study was conducted in accordance with the ethical principles outlined in the World Medical Association's Declaration of Helsinki and received approval from the hospital's ethical committee. Informed consent was obtained from each participant who was informed of her/his right to withdraw from the study at any time without penalty. Anonymity and confidentiality of the information were maintained by storing data on a password-protected computer.
Conflicts of interest
The authors declared no conflict of interest.
Author contributions
OOA: Conceptualization, writing review, writing original draft preparation, and data analysis, supervision; PAA: Conceptualization, writing review, data collection, analysis and validation; OAA: Conceptualization, project administration, editing, supervision, funding acquisition, and validation; KAA: Data collection, critical revision of the article; SOM: Conceptualization, critical revision of the article; SGO: Critical revision of the article; JIA: Data analysis and interpretation, project administration, editing; TFA: Data collection, critical revision of the article; ROF: Critical revision of the article, project administration and editing. All authors read and approved the final manuscript.
Full-Text: (330 Views)
Introduction
Sickle Cell Disease (SCD) remains one of the monogenic disorders of public health importance around the world today owing to its high morbidity and mortality rates (1). It accounts for an estimated 300,000-400,000 live births worldwide and mostly affects Sub-Saharan Africa as compared to other regions (2). According to estimates, the average birth prevalence of homozygous sickle cell disease (HbSS) and sickle cell hemoglobin C disease (HbSC) in Nigeria was 1.21% and 0.24%, respectively, and about 4.2% of national under-5 mortality has been attributed to excess mortality from SCD (3).
Alterations in the form of red blood cells (RBCs) are a hallmark of SCD, a genetic anomaly of the hemoglobin (Hb) molecule that has serious repercussions, including a lower quality of life and a shorter lifespan (4). Clinically, severe hemolysis and abrupt vasoocclusive episodes which cause severe acute and chronic end-organ ischemia and damage, are the major clinical signs of SCD (5,6).
The prevalence of SCD around the globe remains high owing to voluntary population migrations, which allow carriers of the HbS gene to move from one country to another (7). In the past four decades, global health initiatives, including universal newborn screening, vaccines, hydroxyurea therapy, and penicillin prophylaxis, have significantly reduced the morbidity and mortality of children with SCD and its associated mortality in high-income countries (8).
The World Health Organization (WHO) designated hemoglobinopathies, including SCD, as a global public health concern and challenged the national health systems to develop and implement programs for SCD early detection and treatment after issuing a clear call to action in 2006 on how to address the issue globally (7,9). Since then, significant progress has not been made in some regions of the world, especially in high malaria endemic regions, including the Middle East, the Indian subcontinent, some Mediterranean countries, and Sub-Saharan African countries such as Nigeria (5). Meanwhile, SCD often requires hospitalization and multidisciplinary care owing to the numerous associated complications, including but not limited to vasoocclusive crisis (VOC), and respiratory manifestations that cause a progressive decline in lung function (10).
To date, several multidisciplinary approaches have also been formulated for the comprehensive care of people living with SCD. This comprehensive care addresses issues relating to the provision of acute treatment, prevention of complications, emotional assistance for effective coping, and optimal wellness maintenance. An important component of prevention that has been a standard in advanced countries like the USA and a few African countries is the newborn screening program aimed at early detection and reducing the risk of passing the disease to upcoming generations (11,12). National initiatives that improve access to comprehensive treatment, including immunization, prophylactic antibiotics, and pain management techniques with hydroxyurea have also been established as a result of the efforts of the WHO (5).
Several factors in advanced countries have been reportedly responsible for the delivery of effective sickle cell care by health practitioners. A study conducted at John Hopkins demonstrated the significant positive impact that dedicated SCD centers have on rates of ED admission, with a 7% annual reduction in the possibility of readmissions (13). The majority of African countries, including Nigerian healthcare facilities, lack dedicated spaces for interdisciplinary, specialized collaborative, and multifaceted treatment necessary for optimal SCD management (14,15); thereby increasing the frequency of hospital visits and the cost of healthcare for the patients.
Despite the significant strides made to reduce the burden of SCD in Africa, there exists a growing concern about how to address the disparity in the management of acute and chronic complications of the disease in low-resource countries, owing to poorer health outcomes (12). The management of SCD complications and hallmark symptoms has received significant advancement in developed countries with the introduction of global newborn screening initiatives and routine antimicrobial prophylaxis, expansion of treatment, and curative alternatives (5,12). However, its success remains a challenge in developing countries in Sub-Saharan Africa. Importantly, there is still a paucity of literature on challenges encountered in providing care from the health providers’ perspectives, despite the increasing mortality associated with SCD in Nigeria. Evidence-based care on challenges of SCD management from high-income countries showed that sickle cell care can be influenced by the health providers' training, specialization, and practice environment, leaving most patients dissatisfied with the quality of care received from nurses (16). To address this important knowledge gap, understanding the challenges to the care of patients with SCD will enhance improved patients’ outcomes and minimize the frequency of hospital admission. Therefore, the study seeks to understand the challenges faced by nurses in the management of SCD in one of the largest State-owned teaching hospitals in South-west Nigeria. The specific objectives of the study were to identify factors associated with the challenges to SCD care and identify important strategies that can improve care delivery of patients with SCD in the setting.
Methods
Study design
This is a cross-sectional study conducted among nurses working at Osun State University Teaching Hospital in Osogbo, Nigeria, Africa, assessing the challenges they face in managing patients with SCD and the associated factors. It is one of the state-owned tertiary hospitals in South-west Nigeria that offers referral services to neighboring states, including Oyo, Ekiti, and Ondo. The hospital has a 1,120 people, 350 of whom are nurses, with over 1,000 bed capacity. The study was reported in accordance with the STROBE guidelines for strengthening the reporting of observational studies in epidemiology (17).
The sample size was calculated using the Taro Yamane algorithm to estimate the sample size of a known population.
.PNG)
Where; n= sample size, N=population size, e = constant value (0.05) level of precision. The number of nurses working in the hospitals and in specific units where patients with SCD are transferred or admitted is 392; therefore, the required sample size was calculated to be 198, which, taking into account a 10% attrition rate, resulted in a final estimated sample size of 220.
The participants were selected by simple random sampling technique using computer-generated random numbers to ensure equal representation of samples and minimize bias.
The study was conducted among nurses providing care to patients with SCD across various units and wards of the hospital from August 2022 to October 2022. Due to the routine practice of rotating nurses across different units and departments of the hospital, nurses working in the medical and surgical wards, general outpatient department and National Health Insurance outpatient clinic, as well as accident and emergency units, were also recruited. Nurses who met all the following inclusion criteria were recruited: (1) Nurses on full-time employment at the hospital, who mostly partake in the day-to-day care of patients with SCD; (2) Those with at least six months of work experience in providing care to patients with SCD; and (3) Nurses who voluntarily gave informed consent to participate. The exclusion criteria were (1) Nurses involved in various managerial roles which limited their direct contact with patients living with SCD; (2) Those with less than six months of work experience, as they may have limited experience of the challenges involved in SCD management; and (3) Unwillingness to give informed consent.
Study instrument
The instrument for data collection comprised a mix of standardized validated and self-designed questionnaires, divided into four sections A-D. Section A comprised of sociodemographic characteristics of the respondents with five questions, elicited information to describe the sample by age, gender, religion, marital status, and years of practice experience. Section B on the challenges encountered by nurses in managing patients with SCD was measured with the General Clinician Attitudinal rating scale (18), which was adapted with modifications to suit the context of this study. The scale comprises 17 items that measure attitudes and beliefs toward adult patients with SCD using Likert-type items. The scale is composed of four subscales that measure negative attitudes, positive attitudes, concern-raising behaviors, and red-flag behaviors. Internal consistency reliabilities have been reported to range from 0.76-0.89 in previous studies (19,20). The newly modified scale comprising 15-item questions was graded on a four-point Likert scale, with a maximum score of 60 and a minimum score of 15. A favorable reaction was indicated by "Agree or strongly agree", whereas a negative response implies "Disagree or strongly disagree" A high score (Between 31 and 60) indicates an intense challenge in managing patients with SCD, whereas a low score (Between 1 and 30) indicates a diminished level of challenges. The modified instrument was validated for content and reliability index. The internal consistency of the modified instrument had a Cronbach alpha value of 0.88 for total item correlation. Section C on factors associated with challenges experienced in SCD management comprising 6-item questions was measured at a nominal level as a "yes or no" response. Furthermore, section D considered the respondent's perceived strategies that could improve care delivery of patients with SCD in the setting, comprising 6-item questions measured on a 4-point Likert scale, ranging from strongly agree to strongly disagree, with a minimum and maximum score of 6 and 24, respectively. A higher score indicates participants’ perception of various measures for improved care delivery to patients with SCD, while a relatively lower score indicates the least strategies for improved care.
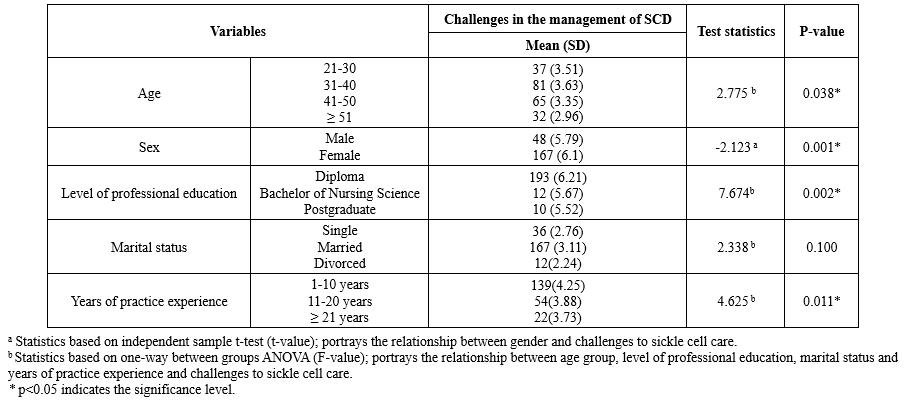
Statistical analysis
The results are presented using frequency distribution with numbers and percentages for categorical data, and mean and standard deviation (SD) for continuous measures. Age, gender, level of professional education, marital status, and years of practice experience were all analyzed as categorical data. Three categories were ultimately established for professional education: diploma, bachelor of nursing science, and postgraduate. The group differences for challenges experienced were compared using an analysis of variance (ANOVA) or independent sample t-test, which was done to determine the relationship between demographic profiles and challenges of managing SCD in the hospital. Assumption for conducting ANOVA was tested using Shapiro-Wilk test. Following the significant one-way ANOVA results, post hoc multiple comparisons were performed using the Tukey honestly significant difference (HSD) test to identify which specific group differed from the others. Data were analyzed with SPSS version 27 at a significant level of 0.05.
Results
A total of 215 responses were received of which five incomplete and improperly filled questionnaires were excluded, resulting in a response rate of 97.7%. Table 1 shows that the majority of respondents, 82 (38.1%), were aged between 31 and 40 years. The mean age of the participants was 24.3 ± 0.94 years. Most participants were female, accounting for 167 (77.7%) of the total. Additionally, the majority of respondents, 193 (89.8%), had a diploma as their highest level of education. Furthermore, 167 (77.7%) of the nurses were married, and 139 (64.7%) had between 1 and 10 years of work experience.
Table 2 indicates the challenges faced by nurses in managing patients with SCD. A good number of the respondents 157 (73%) indicated that patient’s behavior such as failing to comply with medical advice was a challenge. More than half of the respondents, 126 (58.6%), agreed with overcrowding arising from overpopulation of the department, and the most significant 174 (80.9%) expressed challenge was that relating to the addiction of patients to opioids and other analgesics. This is mostly followed by three-fourths of respondents expressing concerns about patients ringing the bell for the nurse and constantly asking for more pain medication before the next due dose, 162 (75.4%). Although some respondents 157 (73%) agreed that many of the patients are drug-seeking when they come into the hospital, more than half 148 (68.9%) agreed that patients always have a history of disputes with staff.
However, most nurses, 180 (83.7%), do not see patients having a history of signing out against medical advice or tampering with a patient-controlled analgesia device 153 (71.1%) and see patients as being frustrating to take care of as a significant challenge 147 (68.4%). Furthermore, most of the respondents disagreed with red flag behaviors as associated challenges in the management of SCD; while negative behaviors and concern-raising behaviors were mostly related to challenges for effective management.
Factors associated with challenges toward management of SCD
Figure 1 shows the factors associated with challenges in managing patients with SCD. Almost all the respondents, 194 (90.2%), stated that lack of financial resources to initiate treatment was a challenge, while more than, half 172 (80%) and 170 (79.1%), pointed to inadequate follow-up of patients with SCD and sociocultural background of the patients, respectively. The least encountered challenge with SCD care was the lack of proper history taking, 136 (63.3%).
Figure 2 shows that the most commonly reported strategy for improving care delivery for patients with SCD in this setting, at 88.4%, was having a coordinated team approach with a nurse specialist as the team leader. Conversely, the least-indicated strategy, at 69.3%, was increasing the number of healthcare professionals involved in SCD management.
Sickle Cell Disease (SCD) remains one of the monogenic disorders of public health importance around the world today owing to its high morbidity and mortality rates (1). It accounts for an estimated 300,000-400,000 live births worldwide and mostly affects Sub-Saharan Africa as compared to other regions (2). According to estimates, the average birth prevalence of homozygous sickle cell disease (HbSS) and sickle cell hemoglobin C disease (HbSC) in Nigeria was 1.21% and 0.24%, respectively, and about 4.2% of national under-5 mortality has been attributed to excess mortality from SCD (3).
Alterations in the form of red blood cells (RBCs) are a hallmark of SCD, a genetic anomaly of the hemoglobin (Hb) molecule that has serious repercussions, including a lower quality of life and a shorter lifespan (4). Clinically, severe hemolysis and abrupt vasoocclusive episodes which cause severe acute and chronic end-organ ischemia and damage, are the major clinical signs of SCD (5,6).
The prevalence of SCD around the globe remains high owing to voluntary population migrations, which allow carriers of the HbS gene to move from one country to another (7). In the past four decades, global health initiatives, including universal newborn screening, vaccines, hydroxyurea therapy, and penicillin prophylaxis, have significantly reduced the morbidity and mortality of children with SCD and its associated mortality in high-income countries (8).
The World Health Organization (WHO) designated hemoglobinopathies, including SCD, as a global public health concern and challenged the national health systems to develop and implement programs for SCD early detection and treatment after issuing a clear call to action in 2006 on how to address the issue globally (7,9). Since then, significant progress has not been made in some regions of the world, especially in high malaria endemic regions, including the Middle East, the Indian subcontinent, some Mediterranean countries, and Sub-Saharan African countries such as Nigeria (5). Meanwhile, SCD often requires hospitalization and multidisciplinary care owing to the numerous associated complications, including but not limited to vasoocclusive crisis (VOC), and respiratory manifestations that cause a progressive decline in lung function (10).
To date, several multidisciplinary approaches have also been formulated for the comprehensive care of people living with SCD. This comprehensive care addresses issues relating to the provision of acute treatment, prevention of complications, emotional assistance for effective coping, and optimal wellness maintenance. An important component of prevention that has been a standard in advanced countries like the USA and a few African countries is the newborn screening program aimed at early detection and reducing the risk of passing the disease to upcoming generations (11,12). National initiatives that improve access to comprehensive treatment, including immunization, prophylactic antibiotics, and pain management techniques with hydroxyurea have also been established as a result of the efforts of the WHO (5).
Several factors in advanced countries have been reportedly responsible for the delivery of effective sickle cell care by health practitioners. A study conducted at John Hopkins demonstrated the significant positive impact that dedicated SCD centers have on rates of ED admission, with a 7% annual reduction in the possibility of readmissions (13). The majority of African countries, including Nigerian healthcare facilities, lack dedicated spaces for interdisciplinary, specialized collaborative, and multifaceted treatment necessary for optimal SCD management (14,15); thereby increasing the frequency of hospital visits and the cost of healthcare for the patients.
Despite the significant strides made to reduce the burden of SCD in Africa, there exists a growing concern about how to address the disparity in the management of acute and chronic complications of the disease in low-resource countries, owing to poorer health outcomes (12). The management of SCD complications and hallmark symptoms has received significant advancement in developed countries with the introduction of global newborn screening initiatives and routine antimicrobial prophylaxis, expansion of treatment, and curative alternatives (5,12). However, its success remains a challenge in developing countries in Sub-Saharan Africa. Importantly, there is still a paucity of literature on challenges encountered in providing care from the health providers’ perspectives, despite the increasing mortality associated with SCD in Nigeria. Evidence-based care on challenges of SCD management from high-income countries showed that sickle cell care can be influenced by the health providers' training, specialization, and practice environment, leaving most patients dissatisfied with the quality of care received from nurses (16). To address this important knowledge gap, understanding the challenges to the care of patients with SCD will enhance improved patients’ outcomes and minimize the frequency of hospital admission. Therefore, the study seeks to understand the challenges faced by nurses in the management of SCD in one of the largest State-owned teaching hospitals in South-west Nigeria. The specific objectives of the study were to identify factors associated with the challenges to SCD care and identify important strategies that can improve care delivery of patients with SCD in the setting.
Methods
Study design
This is a cross-sectional study conducted among nurses working at Osun State University Teaching Hospital in Osogbo, Nigeria, Africa, assessing the challenges they face in managing patients with SCD and the associated factors. It is one of the state-owned tertiary hospitals in South-west Nigeria that offers referral services to neighboring states, including Oyo, Ekiti, and Ondo. The hospital has a 1,120 people, 350 of whom are nurses, with over 1,000 bed capacity. The study was reported in accordance with the STROBE guidelines for strengthening the reporting of observational studies in epidemiology (17).
The sample size was calculated using the Taro Yamane algorithm to estimate the sample size of a known population.
.PNG)
Where; n= sample size, N=population size, e = constant value (0.05) level of precision. The number of nurses working in the hospitals and in specific units where patients with SCD are transferred or admitted is 392; therefore, the required sample size was calculated to be 198, which, taking into account a 10% attrition rate, resulted in a final estimated sample size of 220.
The participants were selected by simple random sampling technique using computer-generated random numbers to ensure equal representation of samples and minimize bias.
The study was conducted among nurses providing care to patients with SCD across various units and wards of the hospital from August 2022 to October 2022. Due to the routine practice of rotating nurses across different units and departments of the hospital, nurses working in the medical and surgical wards, general outpatient department and National Health Insurance outpatient clinic, as well as accident and emergency units, were also recruited. Nurses who met all the following inclusion criteria were recruited: (1) Nurses on full-time employment at the hospital, who mostly partake in the day-to-day care of patients with SCD; (2) Those with at least six months of work experience in providing care to patients with SCD; and (3) Nurses who voluntarily gave informed consent to participate. The exclusion criteria were (1) Nurses involved in various managerial roles which limited their direct contact with patients living with SCD; (2) Those with less than six months of work experience, as they may have limited experience of the challenges involved in SCD management; and (3) Unwillingness to give informed consent.
Study instrument
The instrument for data collection comprised a mix of standardized validated and self-designed questionnaires, divided into four sections A-D. Section A comprised of sociodemographic characteristics of the respondents with five questions, elicited information to describe the sample by age, gender, religion, marital status, and years of practice experience. Section B on the challenges encountered by nurses in managing patients with SCD was measured with the General Clinician Attitudinal rating scale (18), which was adapted with modifications to suit the context of this study. The scale comprises 17 items that measure attitudes and beliefs toward adult patients with SCD using Likert-type items. The scale is composed of four subscales that measure negative attitudes, positive attitudes, concern-raising behaviors, and red-flag behaviors. Internal consistency reliabilities have been reported to range from 0.76-0.89 in previous studies (19,20). The newly modified scale comprising 15-item questions was graded on a four-point Likert scale, with a maximum score of 60 and a minimum score of 15. A favorable reaction was indicated by "Agree or strongly agree", whereas a negative response implies "Disagree or strongly disagree" A high score (Between 31 and 60) indicates an intense challenge in managing patients with SCD, whereas a low score (Between 1 and 30) indicates a diminished level of challenges. The modified instrument was validated for content and reliability index. The internal consistency of the modified instrument had a Cronbach alpha value of 0.88 for total item correlation. Section C on factors associated with challenges experienced in SCD management comprising 6-item questions was measured at a nominal level as a "yes or no" response. Furthermore, section D considered the respondent's perceived strategies that could improve care delivery of patients with SCD in the setting, comprising 6-item questions measured on a 4-point Likert scale, ranging from strongly agree to strongly disagree, with a minimum and maximum score of 6 and 24, respectively. A higher score indicates participants’ perception of various measures for improved care delivery to patients with SCD, while a relatively lower score indicates the least strategies for improved care.
Statistical analysis
The results are presented using frequency distribution with numbers and percentages for categorical data, and mean and standard deviation (SD) for continuous measures. Age, gender, level of professional education, marital status, and years of practice experience were all analyzed as categorical data. Three categories were ultimately established for professional education: diploma, bachelor of nursing science, and postgraduate. The group differences for challenges experienced were compared using an analysis of variance (ANOVA) or independent sample t-test, which was done to determine the relationship between demographic profiles and challenges of managing SCD in the hospital. Assumption for conducting ANOVA was tested using Shapiro-Wilk test. Following the significant one-way ANOVA results, post hoc multiple comparisons were performed using the Tukey honestly significant difference (HSD) test to identify which specific group differed from the others. Data were analyzed with SPSS version 27 at a significant level of 0.05.
Results
A total of 215 responses were received of which five incomplete and improperly filled questionnaires were excluded, resulting in a response rate of 97.7%. Table 1 shows that the majority of respondents, 82 (38.1%), were aged between 31 and 40 years. The mean age of the participants was 24.3 ± 0.94 years. Most participants were female, accounting for 167 (77.7%) of the total. Additionally, the majority of respondents, 193 (89.8%), had a diploma as their highest level of education. Furthermore, 167 (77.7%) of the nurses were married, and 139 (64.7%) had between 1 and 10 years of work experience.
Table 2 indicates the challenges faced by nurses in managing patients with SCD. A good number of the respondents 157 (73%) indicated that patient’s behavior such as failing to comply with medical advice was a challenge. More than half of the respondents, 126 (58.6%), agreed with overcrowding arising from overpopulation of the department, and the most significant 174 (80.9%) expressed challenge was that relating to the addiction of patients to opioids and other analgesics. This is mostly followed by three-fourths of respondents expressing concerns about patients ringing the bell for the nurse and constantly asking for more pain medication before the next due dose, 162 (75.4%). Although some respondents 157 (73%) agreed that many of the patients are drug-seeking when they come into the hospital, more than half 148 (68.9%) agreed that patients always have a history of disputes with staff.
However, most nurses, 180 (83.7%), do not see patients having a history of signing out against medical advice or tampering with a patient-controlled analgesia device 153 (71.1%) and see patients as being frustrating to take care of as a significant challenge 147 (68.4%). Furthermore, most of the respondents disagreed with red flag behaviors as associated challenges in the management of SCD; while negative behaviors and concern-raising behaviors were mostly related to challenges for effective management.
Factors associated with challenges toward management of SCD
Figure 1 shows the factors associated with challenges in managing patients with SCD. Almost all the respondents, 194 (90.2%), stated that lack of financial resources to initiate treatment was a challenge, while more than, half 172 (80%) and 170 (79.1%), pointed to inadequate follow-up of patients with SCD and sociocultural background of the patients, respectively. The least encountered challenge with SCD care was the lack of proper history taking, 136 (63.3%).
Figure 2 shows that the most commonly reported strategy for improving care delivery for patients with SCD in this setting, at 88.4%, was having a coordinated team approach with a nurse specialist as the team leader. Conversely, the least-indicated strategy, at 69.3%, was increasing the number of healthcare professionals involved in SCD management.
Table 3 shows the relationship between the respondents’ characteristics and challenges encountered in the management of Patients with SCD. The challenges varied significantly based on respondents' age (F (3.63) = 2.775, P = 0.038), and years of work experience (F (4.25) = 4.625, P = 0.011. Post hoc analysis in Table 4 shows that respondents within the age range of 21-30 up to 31-40 years were more likely to experience challenges in managing patients with SCD compared to other age groups (P = 0.03). Regarding the years of practice experience, nurses within 1-10 years of work experience had a significant chance of experiencing challenges, compared to those with greater than 21 years of practice experience (P = 0.01).
Similarly, challenges varied based on respondents' level of professional education, as the mean challenge score of those who had diploma certificates (F (6.21) = 7.674, P = 0.002) was significantly higher than those who had bachelor of science (BSc) in nursing and post-graduate degrees. Post hoc analysis revealed that respondents with increasing professional education were less likely to experience challenges in caring for patients with SCD, as those with diploma and BSc in nursing were likely to experience greater challenges (P = 0.00).
Additionally, those who were married showed no significantly higher challenge (M = 167, SD = 3.11) in comparison to the single M=36 (SD=2.76) and divorced nurses M= 12(SD=2.24) (M = 6.42, SD = 6.1; t (128) = 2.338, P = 0.100). Furthermore, the female gender showed a significantly higher challenge in managing patients with SCD with a means score (M) of 167, SD = 6.1; than the males (M = 39, SD = 5.79; t (128) = −2.123, P = 0.001).
Similarly, challenges varied based on respondents' level of professional education, as the mean challenge score of those who had diploma certificates (F (6.21) = 7.674, P = 0.002) was significantly higher than those who had bachelor of science (BSc) in nursing and post-graduate degrees. Post hoc analysis revealed that respondents with increasing professional education were less likely to experience challenges in caring for patients with SCD, as those with diploma and BSc in nursing were likely to experience greater challenges (P = 0.00).
Additionally, those who were married showed no significantly higher challenge (M = 167, SD = 3.11) in comparison to the single M=36 (SD=2.76) and divorced nurses M= 12(SD=2.24) (M = 6.42, SD = 6.1; t (128) = 2.338, P = 0.100). Furthermore, the female gender showed a significantly higher challenge in managing patients with SCD with a means score (M) of 167, SD = 6.1; than the males (M = 39, SD = 5.79; t (128) = −2.123, P = 0.001).
Discussion
The findings of this study provide important insight into the several multifactorial challenges faced by nurses in the management of patients with SCD in a Nigerian hospital setting. Nurses in this study reported a variety of obstacles that are mostly patients and systems-related, including behavior and non-compliance to treatment, opioid addiction in pain management, sickle cell unit congestion and overcrowding, drug-seeking behaviors, and patient-staff disputes. Some of the difficulties the research participants faced are comparable to those that have been previously reported in published evidence-based scholarly articles (21-23). In the context of SCD management, understanding nurses' demographic characteristics is crucial to gaining adequate insight into how they address the challenges associated with this ailment. Most of the respondents in this study fall within the age range of 31-40 years with a mean age of 24.3 years. This age distribution affirms that the hospital's staff is comparatively young, which could affect their training and expertise in treating chronic illnesses like SCD. A younger workforce might be more up-to-date on the latest developments in healthcare procedures, but they might also lack the knowledge and experience necessary to handle complicated medical situations, such as long-term SCD management that necessitates multidisciplinary collaboration (22).
The most significant challenges considered to be associated with patients' negative behaviors as identified by the respondents were those relating to failure to comply with medical advice, with 73.1% of respondents reporting this as an issue, and 80.9% pointing to addiction of patients with SCD to opioids and other analgesics. Non-compliance in chronic conditions such as SCD can arise from various factors, including a lack of understanding of the disease and its severity, the chronic nature of the illness, or psychological factors such as worry or fear of treatment (22). The results of this study are consistent with another Nigerian study (24) that found non-adherence to therapy as a common occurrence among patients with SCD, frequently brought on by misunderstandings about the illness or the adverse effects of drugs. Poorer health outcomes, worsening symptoms, and maybe more frequent hospitalizations can result from patient non-compliance. Noteworthy, a crucial component of therapy for people with SCD is alleviating pain, especially during sickle cell crises. However, the risk of opiate addiction makes it more difficult to manage pain in these people. Nurses in our study expressed concerns that some patients often misuse pain medications, evidenced by some of the patients' ringing bells for nurses’ attention, to request additional pain medications before the next due dose. This mostly complicates treatment regimens, making treatment plans more difficult. Some researchers support this issue by highlighting the difficulties in controlling pain in patients with SCD while also addressing opioid dependence concerns (25,26). Opioid abuse can make it difficult to strike the right balance between pain management and dependency risk; thereby necessitating careful and more sophisticated nursing intervention.
Overcrowding and patient-staff conflicts were also mentioned by our participants as major challenges, with 58.6% and 68.9% of them citing them as such, respectively. This issue is prevalent in many low-resource hospitals where a high volume of patients, limited bed spaces, and insufficient personnel put an additional burden on medical professionals. This problem could have been aggravated by a lack of specialized clinics, specifically built for the care of patients with SCD (27). A previous study shows that in Nigeria's emergency tertiary hospitals, overcrowding and bed shortages have been serious health problems for over a decade (28). Overcrowding increases the rates of nurse turnover, resulting in lower quality of care because nurses are frequently overworked and unable to give individualized care, which is especially important for managing chronic conditions such as patients with SCD who need close observation (29). The patients' discontent with care or displeasure with how their pain is managed may be the cause of the conflicts our study found. Consistent with the findings of other studies, disagreements between patients and medical professionals might cause a communication breakdown, which can affect the nurse-patient relationship (25,30). The ability to provide appropriate treatment may be further hampered by this strain since managing chronic disorders like SCD requires cooperation and confidence.
The findings of this study also showed the factors associated with the challenges experienced by nurses. The most common obstacle, as reported by 90.2% of the participants, was insufficient funds to begin therapy. This aligns with the results of earlier studies that have identified financial limitations as the primary barrier to providing quality healthcare in environments with few resources, such as Nigeria (22,24). Insufficient funds negatively impact patients’ ability to receive blood transfusions, necessary drugs such as opioids, and other supportive therapies needed to control SCD symptoms (21,26). This financial strain may result in inadequate or postponed treatment, which would impair patient outcomes and raise the system's and families' overall healthcare costs.
Furthermore, over 80% of our respondents identified inadequate follow-up care as another significant factor associated with the challenges of managing patients with SCD. Intermittent trips to healthcare professionals and inadequate monitoring of patient's health status are common issues in managing chronic conditions like SCD. However, this could be exacerbated by financial constraints that limit patients' adherence to the usage of health facilities (24). Also, worthy of note is the 63.3% of respondents who acknowledged a lack of proper history taking as the least common challenge. This number emphasizes a crucial component of patient care even though it is lower than the other factors. Adequate history-taking is fundamental for accurate diagnosis, treatment planning, and monitoring of disease progression (31). Incomplete or improper pre-consultation history taking can result in mismanagement, delayed diagnoses, and unnecessary complications (32). This implies that while taking a patient's history may not present as much of a problem as financial considerations, it is still a crucial component of care that cannot be disregarded. Improving patients’ education, expanding access to affordable healthcare, and incorporating sociocultural factors into treatment regimens should be the main goals of initiatives to address these issues. Therefore, the findings of this study support the necessity for a comprehensive strategy in tackling the difficulties of managing chronic conditions like SCD and are in line with the larger body of literature.
While this study assessed the challenges experienced by nurses in managing patients with SCD, utilization of a single site setting in Southwest Nigeria, which does not allow for comparison between two or more settings was a study limitation. This could compromise external validity by making it challenging to extrapolate results to different contexts where problems might be different. Future studies could include responses from diverse settings, with a mix of different professionals’ perspectives. Additionally, responses involving self-reports, such as surveys, entail having knowledge and memory of information, which presents a potential for both social desirability and recall biases. There is a plausible hypothesis that some of the nurses might exaggerate or underestimate the challenges faced during SCD management. Notwithstanding the drawbacks, this study may serve as a basis for subsequent initiatives that seek to improve health outcomes and support for patients with SCD.
Conclusion
This study highlights the significant challenges faced by nurses in a Nigerian hospital when caring for patients with SCD, including systemic and patient-related barriers. Key issues such as unit congestion, opioid addiction, patient non-compliance, and resource shortages complicate care delivery. Financial constraints are particularly pressing, hindering access to essential medications and treatments, while overcrowding and inadequate follow-up care further strain the healthcare system. To improve patients’ outcomes in low-resource settings like Nigeria, it is crucial to enhance training for nurses and patients to better understand the disease and treatment regimens. Improving healthcare infrastructure and ensuring the availability of necessary resources will also facilitate effective care delivery. Prioritizing the alleviation of financial constraints is essential for effective SCD treatment. Continuous educational training for patients can help reduce opioid addiction and promote adherence to treatment. Additionally, targeted training programs for nurses can address systemic issues, ultimately leading to improved patient care and health outcomes.
Acknowledgement
The research team appreciates the valuable contribution of the nurses for their time in participating in this study.
Funding sources
None declared.
Ethical statement
Written permission was obtained from the hospital where the nurses were recruited, with protocol number UTH/EC/2022/10/657. The study was conducted in accordance with the ethical principles outlined in the World Medical Association's Declaration of Helsinki and received approval from the hospital's ethical committee. Informed consent was obtained from each participant who was informed of her/his right to withdraw from the study at any time without penalty. Anonymity and confidentiality of the information were maintained by storing data on a password-protected computer.
Conflicts of interest
The authors declared no conflict of interest.
Author contributions
OOA: Conceptualization, writing review, writing original draft preparation, and data analysis, supervision; PAA: Conceptualization, writing review, data collection, analysis and validation; OAA: Conceptualization, project administration, editing, supervision, funding acquisition, and validation; KAA: Data collection, critical revision of the article; SOM: Conceptualization, critical revision of the article; SGO: Critical revision of the article; JIA: Data analysis and interpretation, project administration, editing; TFA: Data collection, critical revision of the article; ROF: Critical revision of the article, project administration and editing. All authors read and approved the final manuscript.
Type of study: Original Article |
Subject:
Nursing
References
1. Jonathan A, Tutuba H, Lloyd W, Ndunguru J, Makani J, Ruggajo P, et al. Healthcare Workers' Knowledge and Resource Availability for Care of Sickle Cell Disease in Dar es Salaam, Tanzania. Front Genet. 2022;12:773207. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Kato GJ, Piel FB, Reid CD, Gaston MH, Ohene-Frempong K, Krishnamurti L, et al. Sickle cell disease. Nat Rev Dis Primers. 2018;4(1):18010. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Nnodu OE, Oron AP, Sopekan A, Akaba GO, Piel FB, Chao DL. Child mortality from sickle cell disease in Nigeria: a model-estimated, population-level analysis of data from the 2018 Demographic and Health Survey. Lancet Haematol. 2021;8(10):e723-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Elendu C, Amaechi DC, Alakwe-Ojimba CE, Elendu TC, Elendu RC, Ayabazu CP, et al. Understanding Sickle cell disease: Causes, symptoms, and treatment options. Medicine (Baltimore). 2023;102(38):e35237. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Kumar A, Bhattacharya S. Sickle cell disease: a comparative perspective on global and national initiatives. Front Hematol. 2024;3:1457158. [View at Publisher] [DOI] [Google Scholar]
6. Sundd P, Gladwin MT, Novelli EM. Pathophysiology of sickle cell disease. Annu Rev Pathol. 2019:14:263-92. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Russo G, De Franceschi L, Colombatti R, Rigano P, Perrotta S, Voi V, et al. Current challenges in the management of patients with sickle cell disease-A report of the Italian experience. Orphanet J Rare Dis. 2019;14(1):120. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Dexter D, McGann PT. Hydroxyurea for children with sickle cell disease in sub-Saharan Africa: A summary of the evidence, opportunities, and challenges. Pharmacotherapy. 2023;43(5):430-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Kavanagh PL, Fasipe TA, Wun T. Sickle cell disease: a review. JAMA. 2022;328(1):57-68. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Grigoli L, Marocchi M, Venditto L, Piazza M, Tenero L, Piacentini G, et al. Respiratory manifestations of sickle cell disease in children: a comprehensive review for the pediatrician. Expert Rev Respir Med. 2025;19(1):55-71. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Green NS, Zapfel A, Nnodu OE, Franklin P, Tubman VN, Chirande L, et al. The Consortium on Newborn Screening in Africa for sickle cell disease: study rationale and methodology. Blood Adv. 2022;6(24):6187-97. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Dua M, Bello-Manga H, Carroll YM, Galadanci AA, Ibrahim UA, King AA, et al. Strategies to increase access to basic sickle cell disease care in low- and middle-income countries. Expert Rev Hematol. 2022;15(4):333-44. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Lanzkron S, Carroll CP, Hill P, David M, Paul N, Haywood Jr C. Impact of a dedicated infusion clinic for acute management of adults with sickle cell pain crisis. Am J Hematol. 2015;90(5):376-80. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Isa H, Okocha E, Adegoke SA, Nnebe-Agumadu U, Kuliya-Gwarzo A, Sopekan A, et al. Strategies to improve healthcare services for patients with sickle cell disease in Nigeria: The perspectives of stakeholders. Front Genet. 2023;14:1052444. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Adewoyin AS. Management of sickle cell disease: a review for physician education in Nigeria (sub-saharan Africa). Anemia. 2015;2015:791498. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Smeltzer MP, Howell KE, Treadwell M, Preiss L, King AA, Glassberg JA, et al. Identifying barriers to evidence-based care for sickle cell disease: results from the Sickle Cell Disease Implementation Consortium cross-sectional survey of healthcare providers in the USA. BMJ Open. 2021;11(11):e050880. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31-4. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Haywood C, Lanzkron S, Hughes MT, Brown R, Massa M, Ratanawongsa N, et al. A video-intervention to improve clinician attitudes toward patients with sickle cell disease: the results of a randomized experiment. J Gen Intern Med. 2011;26(5):518-23. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Ratanawongsa N, Haywood C, Jr., Bediako SM, Lattimer L, Lanzkron S, Hill PM, et al. Health care provider attitudes toward patients with acute vaso-occlusive crisis due to sickle cell disease: development of a scale. Patient Educ Couns. 2009;76(2):272-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Freiermuth CE, Haywood C, Jr., Silva S, Cline DM, Kayle M, Sullivan D, et al. Attitudes toward patients with sickle cell disease in a multicenter sample of emergency department providers. Adv Emerg Nurs J. 2014;36(4):335-47. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Crosby LE, Quinn CT, Kalinyak KA. A Biopsychosocial Model for the Management of Patients With Sickle-Cell Disease Transitioning to Adult Medical Care. Adv Ther. 2015;32(4):293-305. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Phillips S, Chen Y, Masese R, Noisette L, Jordan K, Jacobs S, et al. Perspectives of individuals with sickle cell disease on barriers to care. PLoS One. 2022;17(3):e0265342. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Druye A, Agyare D, Akoto-Buabeng W, Zutah J, Frank Offei O, Nabe B, et al. Healthcare Professionals' Knowledge, Attitude, Practices of Assessment, and Management of Sickle-Cell Disease: A Meta-Aggregative Review. Diseases. 2024;12(7):156. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Adekunle W, Olaniyan F, Ismail W, Adeyinka J. Assessment of drug adherence among sickle cell disease patients attending secondary health care facility at Ibadan, south west Nigeria. Nigerian Journal of Family Practice. 2019;10(1):39-48. [View at Publisher] [Google Scholar]
25. Osborne JC, Osakwe Z, Odlum M. Opioid use in adults with sickle cell disease hospitalized during vaso-occlusive crisis: a systematic review. J Hematol. 2021;10(2):46-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Sagi V, Mittal A, Tran H, Gupta K. Pain in sickle cell disease: current and potential translational therapies. Transl Res. 2021;234:141-58. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Alshabanat A, Alrabiah M, Bin Zuair A, Aldossari S, Alhumaidi RA. Predictive Factors for 30-Day Readmission and Increased Healthcare Utilization in Sickle Cell Disease Patients: A Single-Center Comparative Retrospective Study. Int J Gen Med. 2024:17:2065-2075. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Soyemi TS, Aborode AT. Shortage of hospital bed capacity and overcrowding in emergency tertiary healthcare centers in Nigeria. Ann Med Surg (Lond). 2022:82:104675. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Guerrero J, Alqarni A, Cordero R, Jarrah I, Alhamaid M. Perceived Causes and Effects of Overcrowding Among Nurses in the Emergency Departments of Tertiary Hospitals: A Multicenter Study Perceived Causes and Effects of Overcrowding Among Nurses in the Emergency Departments of Tertiary Hospitals: A Multicenter Study. Risk Manag Healthc Policy. 2024;17:973-82. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Ehwarieme T, Ugboduma M, Josiah U. Pain Coping Strategies Used and Its Perceived Effectiveness Among Patients Attending Sickle Cell Center in Benin City, Edo State, Nigeria. Nur Primary Care. 2021;5(5):1-8. [View at Publisher] [DOI] [Google Scholar]
31. Meyer AND, Giardina TD, Khawaja L, Singh H. Patient and clinician experiences of uncertainty in the diagnostic process: Current understanding and future directions. Patient Educ Couns. 2021;104(11):2606-15. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Zhakhina G, Tapinova K, Kainazarov T, Kanabekova P. Pre-consultation history taking systems and their impact on modern practices: Advantages and limitations. Journal of Clinical Medicine of Kazakhstan. 2023;20(6):26-35. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


.PNG)