Volume 22, Issue 2 (6-2025)
J Res Dev Nurs Midw 2025, 22(2): 23-27 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghorbani B, Simbeye J, Dehghani M, Bahramnezhad F. Intensive care unit nurses’ perceived Barriers to Optimal Pain management: A cross-sectional study in Tanzania. J Res Dev Nurs Midw 2025; 22 (2) :23-27
URL: http://nmj.goums.ac.ir/article-1-1952-en.html
URL: http://nmj.goums.ac.ir/article-1-1952-en.html
1- Nursing Department, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran; Student Research Committee, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
2- Muhimbili Natinal Hospital, Dar es Salaam, Tanzania
3- Red Crescent Society of the Islamic Republic of Iran, Ministry of Health and Medical Education, Research and Technology Office, Tehran, Iran
4- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran ,bahramnezhad@sina.tums.ac.ir
2- Muhimbili Natinal Hospital, Dar es Salaam, Tanzania
3- Red Crescent Society of the Islamic Republic of Iran, Ministry of Health and Medical Education, Research and Technology Office, Tehran, Iran
4- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran ,
Full-Text [PDF 481 kb]
(425 Downloads)
| Abstract (HTML) (1132 Views)
Full-Text: (207 Views)
Introduction
Pain is a public concern among critically ill non-verbal patients in the ICU (1,2). Most patients hospitalized in ICU are unable to report the severity of pain due to cognitive loss, mechanical ventilation, frequent use of sedation and neuromuscular blockade drugs (1,3,4). Undiagnosed and untreated pain has severe consequences among non-verbal patients nursed in the ICU (5), these include prolonged mechanical ventilation days, acquiring ventilator-associated pneumonia (VAP) and increased hospital stay days (1,6). For that reason, inadequate pain management may lead to poor quality of life and an increased mortality rate among critically ill patients (3,7-9).
Critical care nurses are responsible for diagnosing, assessing and delivering appropriate pain treatment to non-verbal patients admitted in ICU (2,10-12). Hence, critical care nurses need to assess and identify early the barriers that may hinder adequate and proper pain management to find the solutions that will lead to the achievement of optimal pain relief among critically ill non-verbal patients in ICU (8,13,14).
Nurses’ perceived barriers toward pain management include; shortage of equipment, work overload, patients’ fear of drug side effects, inadequate skilled critical care nurses, lack of motivation including low salary, role misunderstanding between nurses and physicians and lack of in-service training (15-18). The majority of nurses indicated poor knowledge of pain management as the barrier. For instance, the overall score was 53.4% in Taipei County, Nurse’s Knowledge & Attitudes Survey - Taiwanese version was used (19,20). Consequently, these reasons indicate that more studies need to be conducted on nurses’ perceived barriers regarding pain management.
Regarding critical care services in Tanzania, still, they are only a few regional and national referral hospitals with ICUs. Consequently, there is a scarcity of clear reputable protocols regarding pain management among non-verbal and intubated ICU patients. The tools mostly used for pain assessment in ICU are self-report and abnormal vital signs. Pharmacological interventions are mostly used for pain treatment, which includes Opioids (Morphine, Pethidine and Fentanyl) and NSAIDs (21-24).
Finally, regarding pain management in Tanzania, especially in the area of critical care, there is a scarcity of studies that have assessed the barriers to pain management among critical care nurses (21). Henceforth, the overall reason for conducting this study was to assess the nurse’s barriers regarding pain management in Tanzanian ICU. The main objective of this study was to determine the nurses' barriers regarding pain management in the ICU in Tanzania.
Methods
Study Design: This cross-sectional study was conducted to assess nurses’ perceived barriers regarding pain management among non-verbal patients admitted to ICUs in Tanzania from January to May 2022. The study followed the STROBE cross-sectional reporting guidelines (25).
Eligibility criteria and setting: The sampling frame consisted of critical care nurses working in Tanzanian ICUs. Nurses with a minimum of six months’ experience in Medical, Surgical, Maternity, Orthopedic, Cardiac, and General ICUs were included. All participants were selected using census sampling to minimize sampling bias. Data collection was carried out in four national referral hospitals: Muhimbili National Hospital, Kilimanjaro Christian Medical Centre, Bugando Medical Centre, and Mbeya Referral Hospital. A total of 202 questionnaires were distributed, of which 170 were completed and returned, yielding a response rate of 84.20%.
Instruments: The barrier assessment tool developed by the Eastern Cooperative Oncology Group (ECOG) was used to evaluate nurses' perceived barriers to pain management in the ICU. The questionnaire items were adapted from the Physician Cancer Pain Survey (26). The tool was pilot-tested and reviewed by a panel of seven pain management experts from South Korea. It demonstrated strong internal consistency with a Cronbach’s alpha > 0.70 (26). The questionnaire consisted of 15 items divided into three categories: patient-related barriers (5 questions), medical staff-related barriers (5 questions), and healthcare system-related barriers (5 questions). Responses were recorded on a 4-point Likert scale: 1 = “never”, 2 = “sometimes”, 3 = “often”, and 4 = “always”. For statistical analysis, responses of 1 and 2 were combined as negative (Not a barrier), and responses of 3 and 4 as positive (A barrier).
Demographic data: Data collected included age, gender, years of experience, education level, and ICU type.
Procedure: Closed-ended questionnaires were distributed by the principal investigator after obtaining ethical approval and permission from the hospital authorities. The purpose and implications of the study were clearly explained to participants before obtaining informed consent. Completed questionnaires were returned in sealed envelopes and collected by the principal investigator.
Statistical analysis: Descriptive statistics, including means and standard deviations, were calculated for continuous variables. The normality of variables was assessed using the Shapiro-Wilk test. Non-parametric tests, including the Kruskal-Wallis test, were used to compare mean differences between groups due to non-normal distribution of data. Post-hoc pairwise comparisons were conducted using Dunn’s test with Bonferroni correction when the Kruskal-Wallis test was significant. The Mann-Whitney U test has also been used. A significance level of P < 0.05 was considered statistically significant. Data were analyzed using IBM SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA).
Results
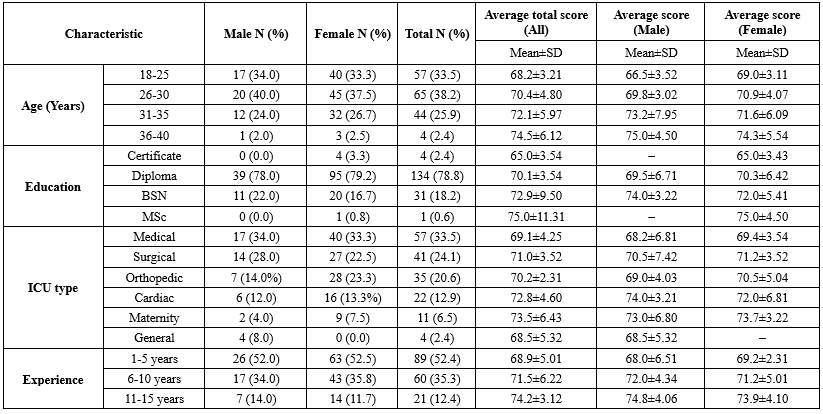
Among 202 nurses involved in this study, 170 nurses completed the questionnaires. The total response rate was 84.20%. The majority of the nurses were between the age of 26-30 years (38.24%) compared to 18-25 years (33.53%). Regarding education majority of the nurses had a diploma in nursing (78.82%). The sample of other demographic characteristics of nurses is highlighted in Table 1.
Nurses' perceived barriers regarding pain management:
The overall mean score of nurses’ perceived barriers to pain management was 10.81 ± 2.21. Medical staff-related barriers showed the highest mean score (4.57 ± 1.24), indicating these were perceived as the most substantial obstacles. Patient-related barriers followed with a mean score of 3.90 ± 1.17, while healthcare system-related barriers were rated lowest (2.33 ± 0.78). Prior to conducting inferential analyses, the normality of the total score variable was assessed using the Shapiro-Wilk test, which revealed a non-normal distribution (P < 0.05). Consequently, non-parametric tests (Kruskal–Wallis) were employed for group comparisons. Gender differences in perceived barriers were analyzed, with results indicating that female nurses reported a higher mean score (10.9 ± 1.75) than male nurses (10.4 ± 2.91). However, the difference was not statistically significant (P = 0.56). With respect to age groups, although some variation in mean scores was observed, the Kruskal-Wallis test indicated that these differences were not statistically significant (H = 0.65, P = 0.88). Analysis by educational level showed that nurses with a diploma in nursing had the highest mean score (11.0 ± 2.02), followed by those with a certificate (10.75 ± 1.50). Nonetheless, the differences in mean scores across educational levels were also not statistically significant (P > 0.05).
Nurses' perceived barriers by professional experience and ICU type
The Kruskal-Wallis test revealed that there were no statistically significant differences in perceived barriers to pain management across nurses' years of experience (P = 0.17).
When analyzed by ICU type, nurses working in the surgical ICU had the highest mean score (11.29 ± 1.64), followed by those working in the cardiac ICU (10.95 ± 2.08). Despite these differences, the Kruskal-Wallis test indicated that they were not statistically significant at the conventional level (P = 0.06) (Table 2).
Pain is a public concern among critically ill non-verbal patients in the ICU (1,2). Most patients hospitalized in ICU are unable to report the severity of pain due to cognitive loss, mechanical ventilation, frequent use of sedation and neuromuscular blockade drugs (1,3,4). Undiagnosed and untreated pain has severe consequences among non-verbal patients nursed in the ICU (5), these include prolonged mechanical ventilation days, acquiring ventilator-associated pneumonia (VAP) and increased hospital stay days (1,6). For that reason, inadequate pain management may lead to poor quality of life and an increased mortality rate among critically ill patients (3,7-9).
Critical care nurses are responsible for diagnosing, assessing and delivering appropriate pain treatment to non-verbal patients admitted in ICU (2,10-12). Hence, critical care nurses need to assess and identify early the barriers that may hinder adequate and proper pain management to find the solutions that will lead to the achievement of optimal pain relief among critically ill non-verbal patients in ICU (8,13,14).
Nurses’ perceived barriers toward pain management include; shortage of equipment, work overload, patients’ fear of drug side effects, inadequate skilled critical care nurses, lack of motivation including low salary, role misunderstanding between nurses and physicians and lack of in-service training (15-18). The majority of nurses indicated poor knowledge of pain management as the barrier. For instance, the overall score was 53.4% in Taipei County, Nurse’s Knowledge & Attitudes Survey - Taiwanese version was used (19,20). Consequently, these reasons indicate that more studies need to be conducted on nurses’ perceived barriers regarding pain management.
Regarding critical care services in Tanzania, still, they are only a few regional and national referral hospitals with ICUs. Consequently, there is a scarcity of clear reputable protocols regarding pain management among non-verbal and intubated ICU patients. The tools mostly used for pain assessment in ICU are self-report and abnormal vital signs. Pharmacological interventions are mostly used for pain treatment, which includes Opioids (Morphine, Pethidine and Fentanyl) and NSAIDs (21-24).
Finally, regarding pain management in Tanzania, especially in the area of critical care, there is a scarcity of studies that have assessed the barriers to pain management among critical care nurses (21). Henceforth, the overall reason for conducting this study was to assess the nurse’s barriers regarding pain management in Tanzanian ICU. The main objective of this study was to determine the nurses' barriers regarding pain management in the ICU in Tanzania.
Methods
Study Design: This cross-sectional study was conducted to assess nurses’ perceived barriers regarding pain management among non-verbal patients admitted to ICUs in Tanzania from January to May 2022. The study followed the STROBE cross-sectional reporting guidelines (25).
Eligibility criteria and setting: The sampling frame consisted of critical care nurses working in Tanzanian ICUs. Nurses with a minimum of six months’ experience in Medical, Surgical, Maternity, Orthopedic, Cardiac, and General ICUs were included. All participants were selected using census sampling to minimize sampling bias. Data collection was carried out in four national referral hospitals: Muhimbili National Hospital, Kilimanjaro Christian Medical Centre, Bugando Medical Centre, and Mbeya Referral Hospital. A total of 202 questionnaires were distributed, of which 170 were completed and returned, yielding a response rate of 84.20%.
Instruments: The barrier assessment tool developed by the Eastern Cooperative Oncology Group (ECOG) was used to evaluate nurses' perceived barriers to pain management in the ICU. The questionnaire items were adapted from the Physician Cancer Pain Survey (26). The tool was pilot-tested and reviewed by a panel of seven pain management experts from South Korea. It demonstrated strong internal consistency with a Cronbach’s alpha > 0.70 (26). The questionnaire consisted of 15 items divided into three categories: patient-related barriers (5 questions), medical staff-related barriers (5 questions), and healthcare system-related barriers (5 questions). Responses were recorded on a 4-point Likert scale: 1 = “never”, 2 = “sometimes”, 3 = “often”, and 4 = “always”. For statistical analysis, responses of 1 and 2 were combined as negative (Not a barrier), and responses of 3 and 4 as positive (A barrier).
Demographic data: Data collected included age, gender, years of experience, education level, and ICU type.
Procedure: Closed-ended questionnaires were distributed by the principal investigator after obtaining ethical approval and permission from the hospital authorities. The purpose and implications of the study were clearly explained to participants before obtaining informed consent. Completed questionnaires were returned in sealed envelopes and collected by the principal investigator.
Statistical analysis: Descriptive statistics, including means and standard deviations, were calculated for continuous variables. The normality of variables was assessed using the Shapiro-Wilk test. Non-parametric tests, including the Kruskal-Wallis test, were used to compare mean differences between groups due to non-normal distribution of data. Post-hoc pairwise comparisons were conducted using Dunn’s test with Bonferroni correction when the Kruskal-Wallis test was significant. The Mann-Whitney U test has also been used. A significance level of P < 0.05 was considered statistically significant. Data were analyzed using IBM SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA).
Results
Among 202 nurses involved in this study, 170 nurses completed the questionnaires. The total response rate was 84.20%. The majority of the nurses were between the age of 26-30 years (38.24%) compared to 18-25 years (33.53%). Regarding education majority of the nurses had a diploma in nursing (78.82%). The sample of other demographic characteristics of nurses is highlighted in Table 1.
Nurses' perceived barriers regarding pain management:
The overall mean score of nurses’ perceived barriers to pain management was 10.81 ± 2.21. Medical staff-related barriers showed the highest mean score (4.57 ± 1.24), indicating these were perceived as the most substantial obstacles. Patient-related barriers followed with a mean score of 3.90 ± 1.17, while healthcare system-related barriers were rated lowest (2.33 ± 0.78). Prior to conducting inferential analyses, the normality of the total score variable was assessed using the Shapiro-Wilk test, which revealed a non-normal distribution (P < 0.05). Consequently, non-parametric tests (Kruskal–Wallis) were employed for group comparisons. Gender differences in perceived barriers were analyzed, with results indicating that female nurses reported a higher mean score (10.9 ± 1.75) than male nurses (10.4 ± 2.91). However, the difference was not statistically significant (P = 0.56). With respect to age groups, although some variation in mean scores was observed, the Kruskal-Wallis test indicated that these differences were not statistically significant (H = 0.65, P = 0.88). Analysis by educational level showed that nurses with a diploma in nursing had the highest mean score (11.0 ± 2.02), followed by those with a certificate (10.75 ± 1.50). Nonetheless, the differences in mean scores across educational levels were also not statistically significant (P > 0.05).
Nurses' perceived barriers by professional experience and ICU type
The Kruskal-Wallis test revealed that there were no statistically significant differences in perceived barriers to pain management across nurses' years of experience (P = 0.17).
When analyzed by ICU type, nurses working in the surgical ICU had the highest mean score (11.29 ± 1.64), followed by those working in the cardiac ICU (10.95 ± 2.08). Despite these differences, the Kruskal-Wallis test indicated that they were not statistically significant at the conventional level (P = 0.06) (Table 2).
|
Table 1. Mean score of nurses’ perceived barriers to pain management
 |
|
Table 2. The ICUs’ nurses perceived barriers towards pain management by demographic characteristics
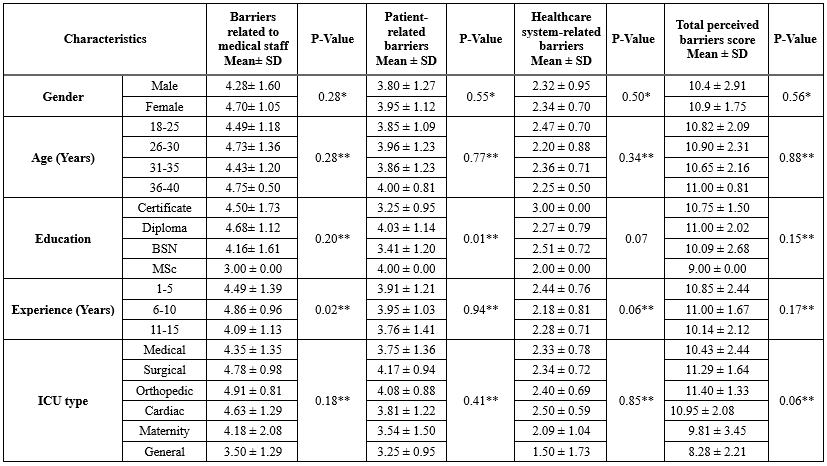 * Mann-Whitney U test ** Kruskal-Wallis test |
Although the result did not reach statistical significance, due to the borderline P-value, a post hoc analysis using pairwise comparisons with Bonferroni correction was considered. However, no pairwise comparison reached statistical significance (P>0.05 in all comparisons), confirming that the observed differences between ICU types were not statistically meaningful (Table 2).
Given the significant result of the Kruskal-Wallis test for patient-related barriers across educational levels (P = 0.01), a post-hoc Dunn’s test with Bonferroni correction was conducted. The results revealed that nurses with diplomas reported significantly higher patient-related barrier scores compared to those with certificates (P = 0.01). Similarly, for barriers related to medical staff by years of experience (P = 0.02), post-hoc analysis showed that nurses with 6-10 years of experience scored significantly higher than those with 11-15 years of experience (P = 0.000).
Discussion
This study aims to assess the critical care nurses’ perceived barriers regarding pain management in Tanzanian ICU. The findings in this study still maintain the barriers related to patients and medical staff as the top major concern in critical care settings in Tanzania.
In this study, critical care nurses in Tanzania demonstrated that barriers related to medical staff were a major obstacle to delivering optimal pain management to critically ill non-verbal patients in the ICU. The majority of nurses participating in the study reported at least one barrier to pain control. These results support other previous study findings that highlighted that insufficient knowledge of control is a huge existing problem among ICU nurses (2,8,10,13,27). This was due to a lack of specific critical care training among bedside ICU nurses working in the ICU but also a lack of in-service training regarding pain management.
Furthermore, this study perceived that there were barriers related to medical staff such as; inadequate experience in pain control, inadequate pain assessment, reluctance to prescribe opioids, Time constraints and insufficient communication with patients. However, this may be due to inadequate knowledge of using behavioral scales among critical care nurses on pain assessment to non-verbal patients (2,8,10). The majority of patients in the ICU are either intubated or non-intubated on non-invasive respiratory support. For that reason, critical care nurses need to have both skills of using pain behavioral assessment scales such as Behavioral Pain Scale (BPS) and Critical-Care Pain Observation Tool (CPOT) for pain assessment to critically ill non-verbal patients (10,14,28-30).
Consequently, in this study, ICU nurses perceived patient-related barriers as an obstacle to providing proper pain management among critically ill non-verbal patients. The findings supported other previous studies which reported insufficient communication with medical staff and reluctance to report pain (13,31,32). This still was due to intubation and impaired cognition among non-verbal patients (30,33). Due to the severity of patients most patients in ICU are unable to report their level of pain intensity to nurses (34-36).
In addition, critical care nurses reported another patient-related barrier which includes reluctance to take opioids, financial constraints and insufficient knowledge of pain control (13,37-39). This might be contributed by limited knowledge regarding the consequences of pain but also the cultural environment (14,40,41). Akbar et al, (2019) explained the integration of cultural preferences on pain management. The author highlighted that religion has more influence on the effectiveness of pain management interventions and may cause patients to refuse to take pain medication (14). Therefore, critical care nurses need to be aware of the culture and religious beliefs of patients during pain assessment to achieve optimal pain management among critically ill non-verbal patients in the ICU (42,43).
Finally, critical care nurses in Tanzania did not perceive barriers related to the healthcare system. These barriers related to the healthcare system include strict regulation of opioids, inadequate staffing and limited stock of different types of opioids. These findings supported previous studies where nurses did not report barriers related to the healthcare system as an obstacle to achieving effective pain management (13,14,40). This was due to the availability of drugs in critical care settings, especially opioids and NSAIDs (Nonsteroidal anti-inflammatory drugs). Not only this but also nurses had no restrictions on using these medications in case they identified that the patient was in pain, however, the specific tools were not used in pain assessment, especially CPOT and BPS (28). This needs to be monitored closely to make sure critical care nurses use specific pain assessment tools for pain management among non-verbal critically ill in order to reduce underestimation and undertreatment of patient’s pain.
The limitations of this study include its sampling and the fact that the sample was limited to four hospitals. Although these four hospitals were government and university referral hospitals in Tanzania, this limitation should be considered in generalizing the findings.
Conclusion
This study explored the perceived barriers to pain management among critical care nurses in the ICU. The majority of nurses identified medical staff-related and patient-related barriers as the primary challenges, while healthcare system-related barriers were not perceived as significant. The findings underscore the need for targeted training programs to improve nurses’ competencies in pain diagnosis, assessment, and management, particularly for non-verbal critically ill patients. The use of validated pain assessment tools such as the behavioral pain scale and critical-care pain observation tool is recommended to enhance pain evaluation accuracy. Early identification and proactive management of barriers by critical care nurses are crucial to achieving optimal pain management outcomes in ICU settings. This competency can be enhanced through continuous professional development, including in-service training, online courses, and advanced nursing education such as a Master’s degree in critical care nursing. Furthermore, hospitals with ICUs should establish and enforce evidence-based policies that support critical care nurses in delivering optimal pain management. Such policies must be inclusive and considerate of patients’ diverse backgrounds, including cultural, religious, and socio-economic factors, to ensure equitable and effective care.
Acknowledgement
The authors are grateful to the ethical research committee of the school of Nursing and Rehabilitation of Tehran University of Medical Sciences, Tehran, Iran, and hereby express their gratitude to all the participating in this study.
Funding sources
None.
Ethical statement
This study received ethical approval from the Research Ethics Committee of the Faculty of Nursing and Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran (IR.TUMS.FNM.REC.1398.150). Although data collection was conducted in Tanzania, the project was scientifically supervised and supported by TUMS. Therefore, in accordance with the university’s policies and ethical standards for research, ethical approval was obtained from the Ethics Committee of Tehran University of Medical Sciences. Our code of ethics has been approved in Tanzania according to University of Tanzania rules, so no new approval is needed. All participants provided written informed consent, and ethical considerations including confidentiality and the right to withdraw were respected throughout the study.
Conflicts of interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Author contributions
BG: Conceptualization, Methodology, Data Analysis, Writing - Original Draft. JS: Investigation, Data Collection, Writing - Review and Editing.
MD: Data Curation, Formal Analysis, Writing - Review and Editing. FB: Supervision, Project Administration, Writing - Review and Final Approval of the Manuscript.
Data availability statement
De-identified data can be obtained from the corresponding author upon a reasonable request.
Given the significant result of the Kruskal-Wallis test for patient-related barriers across educational levels (P = 0.01), a post-hoc Dunn’s test with Bonferroni correction was conducted. The results revealed that nurses with diplomas reported significantly higher patient-related barrier scores compared to those with certificates (P = 0.01). Similarly, for barriers related to medical staff by years of experience (P = 0.02), post-hoc analysis showed that nurses with 6-10 years of experience scored significantly higher than those with 11-15 years of experience (P = 0.000).
Discussion
This study aims to assess the critical care nurses’ perceived barriers regarding pain management in Tanzanian ICU. The findings in this study still maintain the barriers related to patients and medical staff as the top major concern in critical care settings in Tanzania.
In this study, critical care nurses in Tanzania demonstrated that barriers related to medical staff were a major obstacle to delivering optimal pain management to critically ill non-verbal patients in the ICU. The majority of nurses participating in the study reported at least one barrier to pain control. These results support other previous study findings that highlighted that insufficient knowledge of control is a huge existing problem among ICU nurses (2,8,10,13,27). This was due to a lack of specific critical care training among bedside ICU nurses working in the ICU but also a lack of in-service training regarding pain management.
Furthermore, this study perceived that there were barriers related to medical staff such as; inadequate experience in pain control, inadequate pain assessment, reluctance to prescribe opioids, Time constraints and insufficient communication with patients. However, this may be due to inadequate knowledge of using behavioral scales among critical care nurses on pain assessment to non-verbal patients (2,8,10). The majority of patients in the ICU are either intubated or non-intubated on non-invasive respiratory support. For that reason, critical care nurses need to have both skills of using pain behavioral assessment scales such as Behavioral Pain Scale (BPS) and Critical-Care Pain Observation Tool (CPOT) for pain assessment to critically ill non-verbal patients (10,14,28-30).
Consequently, in this study, ICU nurses perceived patient-related barriers as an obstacle to providing proper pain management among critically ill non-verbal patients. The findings supported other previous studies which reported insufficient communication with medical staff and reluctance to report pain (13,31,32). This still was due to intubation and impaired cognition among non-verbal patients (30,33). Due to the severity of patients most patients in ICU are unable to report their level of pain intensity to nurses (34-36).
In addition, critical care nurses reported another patient-related barrier which includes reluctance to take opioids, financial constraints and insufficient knowledge of pain control (13,37-39). This might be contributed by limited knowledge regarding the consequences of pain but also the cultural environment (14,40,41). Akbar et al, (2019) explained the integration of cultural preferences on pain management. The author highlighted that religion has more influence on the effectiveness of pain management interventions and may cause patients to refuse to take pain medication (14). Therefore, critical care nurses need to be aware of the culture and religious beliefs of patients during pain assessment to achieve optimal pain management among critically ill non-verbal patients in the ICU (42,43).
Finally, critical care nurses in Tanzania did not perceive barriers related to the healthcare system. These barriers related to the healthcare system include strict regulation of opioids, inadequate staffing and limited stock of different types of opioids. These findings supported previous studies where nurses did not report barriers related to the healthcare system as an obstacle to achieving effective pain management (13,14,40). This was due to the availability of drugs in critical care settings, especially opioids and NSAIDs (Nonsteroidal anti-inflammatory drugs). Not only this but also nurses had no restrictions on using these medications in case they identified that the patient was in pain, however, the specific tools were not used in pain assessment, especially CPOT and BPS (28). This needs to be monitored closely to make sure critical care nurses use specific pain assessment tools for pain management among non-verbal critically ill in order to reduce underestimation and undertreatment of patient’s pain.
The limitations of this study include its sampling and the fact that the sample was limited to four hospitals. Although these four hospitals were government and university referral hospitals in Tanzania, this limitation should be considered in generalizing the findings.
Conclusion
This study explored the perceived barriers to pain management among critical care nurses in the ICU. The majority of nurses identified medical staff-related and patient-related barriers as the primary challenges, while healthcare system-related barriers were not perceived as significant. The findings underscore the need for targeted training programs to improve nurses’ competencies in pain diagnosis, assessment, and management, particularly for non-verbal critically ill patients. The use of validated pain assessment tools such as the behavioral pain scale and critical-care pain observation tool is recommended to enhance pain evaluation accuracy. Early identification and proactive management of barriers by critical care nurses are crucial to achieving optimal pain management outcomes in ICU settings. This competency can be enhanced through continuous professional development, including in-service training, online courses, and advanced nursing education such as a Master’s degree in critical care nursing. Furthermore, hospitals with ICUs should establish and enforce evidence-based policies that support critical care nurses in delivering optimal pain management. Such policies must be inclusive and considerate of patients’ diverse backgrounds, including cultural, religious, and socio-economic factors, to ensure equitable and effective care.
Acknowledgement
The authors are grateful to the ethical research committee of the school of Nursing and Rehabilitation of Tehran University of Medical Sciences, Tehran, Iran, and hereby express their gratitude to all the participating in this study.
Funding sources
None.
Ethical statement
This study received ethical approval from the Research Ethics Committee of the Faculty of Nursing and Rehabilitation, Tehran University of Medical Sciences, Tehran, Iran (IR.TUMS.FNM.REC.1398.150). Although data collection was conducted in Tanzania, the project was scientifically supervised and supported by TUMS. Therefore, in accordance with the university’s policies and ethical standards for research, ethical approval was obtained from the Ethics Committee of Tehran University of Medical Sciences. Our code of ethics has been approved in Tanzania according to University of Tanzania rules, so no new approval is needed. All participants provided written informed consent, and ethical considerations including confidentiality and the right to withdraw were respected throughout the study.
Conflicts of interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Author contributions
BG: Conceptualization, Methodology, Data Analysis, Writing - Original Draft. JS: Investigation, Data Collection, Writing - Review and Editing.
MD: Data Curation, Formal Analysis, Writing - Review and Editing. FB: Supervision, Project Administration, Writing - Review and Final Approval of the Manuscript.
Data availability statement
De-identified data can be obtained from the corresponding author upon a reasonable request.
Type of study: Original Article |
Subject:
Nursing
References
1. Ayasrah SM. Pain among non-verbal critically Ill mechanically ventilated patients: Prevalence, correlates and predictors. J Crit Care. 2019;49:14-20. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Salim I, Ejheisheh MA, Ayed A, Aqtam I, Batran A. Barriers and practices in pain management for intubated patients: A study of critical care nurses in Southern West Bank hospitals. PloS one. 2025;20(3):e0320430. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Hajiesmaeili MR, Safari S. Pain management in the intensive care unit: do we need special protocols? Anesth Pain Med. 2012;1(4):237-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Bennett S, Hurford WE. When should sedation or neuromuscular blockade be used during mechanical ventilation? Respir Care. 2011;56(2):168-80. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Rani V, Kour P. Attitudes of Nurses Towards Pain Management in Geriatric Care. 2025. [View at Publisher] [Google Scholar]
6. Park J-M, Kim JH. Assessment and treatment of pain in adult intensive care unit patients. The Korean J Crit Care. Med2014;29(3):147-59. [View at Publisher] [DOI] [Google Scholar]
7. Brennan F, Lohman D, Gwyther L. Access to Pain Management as a Human Right. Am J Public Health. 2019;109(1):61-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Batiha A-M. Pain management barriers in critical care units: A qualitative study. International Journal of Advanced Nursing Studies. 2014;3(1):1. [View at Publisher] [DOI] [Google Scholar]
9. Shrestha S, Sapkota S, Teoh SL, Kc B, Paudyal V, Lee SWH, et al. Comprehensive assessment of pain characteristics, quality of life, and pain management in cancer patients: a multi-center cross-sectional study. Qual Life Res. 2024;33(10):2755-71. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Deldar K, Froutan R, Ebadi A. Challenges faced by nurses in using pain assessment scale in patients unable to communicate: a qualitative study. BMC Nurs. 2018;17:11. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Choi J, Campbell ML, Gélinas C, Happ MB, Tate J, Chlan L. Symptom assessment in non-vocal or cognitively impaired ICU patients: implications for practice and future research. Heart Lung. 2017;46(4):239-45. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Zakeri H, Mahtosh P, Radmehr M, Rahbani R, Montazeri L, Moalemi S, et al. Pain Management strategies in Intensive care unit: challenges and Best Practice. Galen Med J. 2024;13:e3264. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. D'emeh WM, Yacoub MI, Darawad MW, Al-Badawi TH, Shahwan B. Pain-related knowledge and barriers among Jordanian nurses: a national study. Health. 2016;8(06):548. [View at Publisher] [DOI] [Google Scholar]
14. Akbar N, Teo SP, Hj-Abdul-Rahman NA, Hj-Husaini A, Venkatasalu MR. Barriers and Solutions for Improving Pain Management Practices in Acute Hospital Settings: Perspectives of Healthcare Practitioners for a Pain-free Hospital Initiative.Ann Geriatr Med Res. 2019;23(4):190-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Darawad M, Alnajar MK, Abdalrahim MS, El-Aqoul AM. Cancer Pain Management at Oncology Units: Comparing Knowledge, Attitudes and Perceived Barriers Between Physicians and Nurses. J Cancer Educ. 2019;34(2):366-74. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Kassa RN, Kassa GM. Nurses' attitude, practice and barrier s toward cancer pain management, Addis Ababa, Ethiopia. J Cancer Sci Ther. 2014;6(12):483-7. [View at Publisher] [DOI] [Google Scholar]
17. Mędrzycka-Dąbrowska W, Dąbrowski S, Gutysz-Wojnicka A, Basiński A, Kwiecień-Jaguś K. Nurses' knowledge and Barriers Regarding Pain Management. J Perianesth Nurs. 2018;33(5):715-26. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Rababa M, Al-Sabbah S, Hayajneh AA. Nurses' Perceived Barriers to and Facilitators of Pain Assessment and Management in Critical care Patients: A Systematic Review. J Pain Res. 2021:14:3475-91. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Wang HL, Tsai YF. Nurses' knowledge and barriers regarding pain management in intensive care units. J Clin Nurs. 2010;19(21‐2):3188-96. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Shoqirat N, Mahasneh D, Al-Khawaldeh O, Al Hadid L. Nurses' Knowledge, Attitudes, and Barriers Toward Pain Management Among Postoperative Patients in Jordan. J Perianesth Nurs. 2019;34(2):359-67. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Samwel R, Boniface R. Pain management and factors associated with its severity among post surgical patients admitted in the intensive care unit at Muhimbili national hospital, Tanzania. Open Journal of Anesthesiology. 2019;9(2):23-33. [View at Publisher] [DOI] [Google Scholar]
22. Tanzania D. Ministry of Health, Community Development, Gender, Elderly and Children. [View at Publisher] [Google Scholar]
23. Fan B. Medication Treatment for Visceral Pain. Visceral Pain: From Bench to Bedside: Springer; 2024. p. 89-98. [View at Publisher] [DOI] [Google Scholar]
24. Sukhram SD, Yilmaz G, Erichsen S, Vassilevich S. Exploring the Efficacy and Safety of Ketamine for Managing Acute Renal Colic in Emergency Departments: A Systematic Review of Recent Clinical Trials. Int J Mol Sci. 2025;26(1):371. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Elm EV, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP,et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. . Bull World Health Organ. 2007;370(9596):1453-57. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA,et al. Pain and its treatment in outpatients with metastatic cance. N Engl J Med. 330(9):592-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Iklima N, Maidartati M, Irawan E, Nurlianawati L, Nuryanti L. Identifying Barriers to Optimal Pain Management in ICU Nurses: A Cross-Sectional Analysis. Journal Medical Informatics Technology. 2025:1-7. [View at Publisher] [DOI] [Google Scholar]
28. Severgnini P, Pelosi P, Contino E, Serafinelli E, Novario R, Chiaranda M. Accuracy of Critical Care Pain Observation Tool and Behavioral Pain Scale to assess pain in critically ill conscious and unconscious patients: prospective, observational study. J Intensive Care. 2016;4:68. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Thomas D, Kuruppasseril AJ, Samad RA, George EJ. Comparative Accuracy of Critical Care Pain Observation Tool (CPOT), Behavioral Pain Scale (BPS), and Non-verbal Pain Scale (NVPS) for Pain Assessment in Mechanically Ventilated Intensive Care Unit Patients: A Prospective Observational Study. Indian J Crit Care Med. 2025;29(6):492-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Wadumanannalage P, Kumara PR, Arachchilage A, Amarasinghe RP. Pain Management in the intensive care. Descriptive literature review. 2025. [View at Publisher] [Google Scholar]
31. Berben SAA, Meijs THJM, van Grunsven PM, Schoonhoven L, van Achterberg T. Facilitators and barriers in pain management for trauma patients in the chain of emergency care. Injury. 2012;43(9):1397-402. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Gerber K, Willmott L, White B, Yates P, Mitchell G, Currow DC, et al. Barriers to adequate pain and symptom relief at the end of life: A qualitative study capturing nurses' perspectives. Collegian. 2022;29(1):1-8. [View at Publisher] [DOI] [Google Scholar]
33. Pu L, Barton M, Kodagoda Gamage M, Okada M, Todorovic M, Moyle W. Pain Assessment and Management in Dementia Care: Qualitative Perspectives of People With Dementia, Their Families, and Healthcare Professionals. J Clin Nurs. 2025;34(7):2933-47. [View at Publisher] [DOI] [PMID] [Google Scholar]
34. Miller EL, Okour A. Pain Management Among the Cognitively Impaired. Pain Manag Nurs. 2024;25(2):101-3. [View at Publisher] [DOI] [PMID] [Google Scholar]
35. Rababa M, Al-Sabbah S. Nurses' Pain Assessment Practices for Cognitively Intact and Impaired Older Adults in Intensive Care Units. Dement Geriatr Cogn Dis Extra. 2022;12(2):115-21. [View at Publisher] [DOI] [PMID] [Google Scholar]
36. Papanikita M, Pavlatou N. Knowledge and attitudes of nurses regarding pain in adults' intensive care units. Health AND Research Journal. 2025;11(1):29-41. [View at Publisher] [DOI] [Google Scholar]
37. Graczyk M, Borkowska A, Krajnik M. Why patients are afraid of opioid analgesics: a study on opioid perception in patients with chronic pain. Pol Arch Intern Med. 2018;128(2):89-97. [View at Publisher] [DOI] [PMID] [Google Scholar]
38. Bulls HW, Hamm M, Wasilko R, de Abril Cameron F, Belin S, Goodin BR, et al. "I Refused to Get Addicted to Opioids": Exploring Attitudes About Opioid Use Disorder in Patients With Advanced Cancer Pain and Their Support People. J Pain. 2023;24(6):1030-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
39. Vranken MJ, Linge-Dahl L, Mantel-Teeuwisse AK, Radbruch L, Schutjens M-HD, Scholten W, et al. The perception of barriers concerning opioid medicines: A survey examining differences between policy makers, healthcare professionals and other stakeholders. Palliat Med. 2020;34(4):493-50. [View at Publisher] [DOI] [PMID] [Google Scholar]
40. Al-Mahrezi A. Towards Effective Pain Management: Breaking the Barriers.Oman Med J. 2017;32(5):357-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
41. Rogger R, Bello C, Romero CS, Urman RD, Luedi MM, Filipovic MG. Cultural Framing and the Impact on Acute Pain and Pain Services. Curr Pain Headache Rep.2023;27(9):429-36. [View at Publisher] [DOI] [PMID] [Google Scholar]
42. Jamal K, Alameri RA, Alqahtani FM, AlGarni RS, Alamri NA, Elshnawie HA, et al. Knowledge and Attitudes of Critical Care Nurses Regarding Pain Management in Saudi Arabia. Med Arch. 2023;77(1):49-55. [View at Publisher] [DOI] [PMID] [Google Scholar]
43. Kuhlmann EH, Tallman BA. The Impact of Nurses' Beliefs, Attitudes, and Cultural Sensitivity on the Management of Patient Pain. J Transcult Nurs. 2022;33(5):624-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |