Volume 22, Issue 2 (6-2025)
J Res Dev Nurs Midw 2025, 22(2): 33-38 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fereidouni Sarijeh P, Khatib A, Salmani S, Fransiz M. The effect of education and telephone follow-up after discharge (telenursing) on care pressure and resilience in caregivers of bipolar patients: A quasi-experimental study. J Res Dev Nurs Midw 2025; 22 (2) :33-38
URL: http://nmj.goums.ac.ir/article-1-1974-en.html
URL: http://nmj.goums.ac.ir/article-1-1974-en.html
1- Department of Nursing, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
2- Department of Nursing, School of Nursing and Midwifery, Neyshabur University of Medical Sciences, Neyshabur, Iran ,Khatiba1@nums.ac.ir
3- Highgate Mental Health Centre, North London NHS Foundation Trust (I&C), London, United Kingdom
4- Department of Public Health, School of Public Health, Ardabil University of Medical Sciences, Ardabil, Iran
2- Department of Nursing, School of Nursing and Midwifery, Neyshabur University of Medical Sciences, Neyshabur, Iran ,
3- Highgate Mental Health Centre, North London NHS Foundation Trust (I&C), London, United Kingdom
4- Department of Public Health, School of Public Health, Ardabil University of Medical Sciences, Ardabil, Iran
Full-Text [PDF 484 kb]
(458 Downloads)
| Abstract (HTML) (1162 Views)
Discussion
The result of the present study showed that the telenursing intervention has an effect on the care pressure and resilience of caregivers of bipolar patients. In line with the results of the present study, different studies have shown the effectiveness of telenursing in decreasing the care pressure of family caregivers of patients with diagnoses of hemodialysis (29), stroke (30), heart failure (31), Alzheimer’s disease, dementia (14), and Covid-19 (32). A study examining the effect of psychological training on the resilience of family caregivers of clients with bipolar disorder showed that psychological training is effective on resilience (12). Another study examined the psychological stress of family caregivers of hospitalized schizophrenia patients. Their findings showed that 12.2% of caregivers had mild, 36.4% had moderate, and 51.4% had severe psychological stress (33). In the present study, caregivers also endured high caregiving stress. Care pressure in the families of patients with bipolar affective disorder was investigated in the other study, which indicated that greater care pressure was associated with longer duration of illness and more life cycles, and care pressure was high in the families of patients with bipolar disorder (34). Care pressure has been reported as a predictor of depression among family and friends caring for people with bipolar disorder (35). In a cross-sectional study, fifty-one patients with bipolar disorder who were attending an outpatient clinic were evaluated. Care pressure among their caregivers was assessed using the Care pressure Assessment Schedule and it was found that caregivers experienced higher care pressure (36).
Telenursing is the use of information and communication technologies to develop all fields of nursing care, education and research at a distance (37). Telenursing is utilized to improve nursing care processes and competencies, lessen time and location-based disparities in nursing care access, and support nursing education, training, and scientific advancement. Since telenursing saves nursing time and resources, allows nurses to provide care, monitoring, and education, wherever and whenever needed, and gives consumers information to encourage self-care (16).
Traditional services are provided by the healthcare system in Iran. Although all complications from traditional methods cannot currently be managed by telenursing, but factors such as access to care, cost-effective delivery and the distribution of scarce providers are well addressed by telenursing. The development of telenursing techniques is actually an attempt to get around the geographical and temporal barriers to care service delivery. Patients receive the care they require as soon as possible, which allow for good spatial control. The chronic nature of heart failure and the need to provide these patients with faster care services make telenursing systems necessary. Patients with heart failure make up a significant percentage of chronic patients (31).
The strengths of the present study include the random selection of the study population and the use of control groups, which was also provided with an educational brochure produced following completion of the study that was a useful guide for caregivers. One of the study's limitations was receiving training and information from other sources that could affected the study's findings, which were partially managed by using a control group. Furthermore, people differed in their capacity to handle crises and issues as well as adjust to them, which may have an effect on unsustainable results.
Conclusion
As evidenced by the results of the present study, education and telephone follow-up after discharge (Telenursing) was positively effective on care pressure and resilience of caregivers of bipolar patients. These results can be used to educate caregivers in different diseases. To confirm and verify the present results, future studies with longer intervention duration should be conducted. Considering the effect of telenursing on reducing caregiver pressure and increasing resilience in caregivers of bipolar patients, this method can also be considered as an auxiliary method for controlling the symptoms.
Acknowledgement
The authors would like to express their gratitude to the respected authorities and families of the patients who participated in this study.
Funding sources
The authors received no financial support for the research, authorship, and/or publication of this article
Ethical statement
This research was approved by the Committee of Ethics in Human Research at Neyshabur University of Medical Sciences (Ethical code: IR.NUMS.REC.1403.059). All participants signed informed written consent after the relevant procedures and the purpose of the study were fully explained. Also, all patients completed all questionnaires. All participants first filled out an informed consent form and then entered the study. All methods were carried out in accordance with the Declaration of Helsinki. All participants’ information was preserved and they had the right to withdraw from the study.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All authors participated in the design and formulation of the study. PF was involved in data collection. AKh prepared the initial draft of the article. PF, AKh, and MF carefully reviewed and revised the research design, data analysis, and interpretation of results. SS participated in the review of the final version of the article. All statistical analyses were performed by the research team and there was no separate statistical consultant involved in this study. All authors read and approved the final version of the article.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Full-Text: (176 Views)
Introduction
Bipolar disorder (BD) is recognized as a multisystem illness affecting mood and cognitive, endocrine, autonomic, and sleep functions (1). According to the World Health Organization (WHO), there are approximately 45 million cases of bipolar disorder worldwide (2). In Iran, the prevalence of BD is 25% to 31% (3,4). Bipolar disorder has been ranked among the most disabling disorders due to its unavoidable and severe consequences, recurrent nature, and high costs. Special attention has been paid to the care and treatment of patients with this disorder and have emphasized the role of families in caring for these patients (5,6). One of the goals of the World Health Organization in promoting mental health and treating mental illnesses in recent years is to reduce the length of hospital stays and expand social services (7). More than 60% of clients who are discharged from mental disorders centers return to their families and receive their complementary care (8).
Families are the primary source of care for people with severe mental disorders. They provide financial, companionship, emotional, and health care support to members of the family with mental disorders at home. However, the development of bipolar disorder in one family member affects the entire family, causing a loss of family coping skills and strength (9). Caring for these patients depletes the family's energy and causes despair, helplessness, depression, exhaustion, and emergence or exacerbation of psychosomatic disorders in other family members, especially the primary caregivers (10). These consequences are more pronounced in individuals who have a greater role in patient’s care (11). As a result, all family members, especially the primary caregiver, experience high levels of caregiving stress, which can cause high levels of stress, depression, and low self-efficacy in caregivers (12). This care pressure depends on the factors such as age and gender of the caregivers, the quality of their previous relationship with the client, the caregivers' assessment of the situation, their perception of the illness, and the coping strategies used by the caregivers. On the other hand, caregivers by resilience can overcome the stress of caring for a client with a mental disorder and maintain their own and their family's health (13).
Resilience means controlling or acting on stressors before they harm the individual; resilient behaviors help individuals overcome negative experiences and transform them into positive ones. The characteristics of resilience include flexibility, tirelessness, self-awareness, and altruism (14). The studies have shown that coping skills training and resilience-building programs produce effective results for clients and their caregivers. Considering the role of families in the care of patients with bipolar disorder, their systematic education has been emphasized (12). Telenursing is a method used to provide remote care services at home, especially for patients who are immobile or live in remote and rural areas, and those with chronic conditions such as chronic obstructive pulmonary disease, diabetes, congenital heart disease, disability and incapacity, and chronic neurological disorders (Parkinson's and Alzheimer's) (15). Telenursing is established through video conferencing, video phone, and the Internet without time or place restrictions; it provides the possibility of educating patients and their families and providing remote consultation and sending educational programs to patients and their relatives via email (16,17).
Caring for a patient with a mental disorder imposes a lot of pressure and stress on family members, which reduces the quality of life in these individuals. Family pressures and stresses may increase the risk of relapse in the patient (18). Telenursing reduced the burden of care for healthcare staff but increased their performance (19). Abdigaravand et al. in 2023 reported the effect of education and telephone follow-up to reduce the burden of caring for families of cancer patients (20). Telephone consultations facilitate patient access, reduce costs, and eliminate time and location barriers (21). Another research indicated that telephone training has reduced the burden of care for healthcare professionals but increased their performance (22). Among all patient education methods, telenursing is a common method to support patients and nurses. It is cost-effective because it prevents readmissions and improves the quality of care. Although research studies have expanded over the past decade, there is an urgent and serious need to strengthen and expand such projects, especially in the development, design, and evaluation of effective family intervention strategies. There is also a continuing need to improve and enhance the level of psychiatric service delivery to severely mentally ill patients and their families (18). In particular, reducing the burden of care and increasing the resilience of family members in caring for a mentally ill patient are essential. Therefore, the present study was conducted with aim to evaluate the effect of education and telephone follow-up after discharge (Telenursing) on care pressure and resilience of caregivers of bipolar patients.
Methods
This quasi-experimental study with a pre-test and post-test design and a control group was conducted from September 2024 to March 2025 at Razi Psychiatric Hospital in Tehran. The statistical population consisted of family caregivers of clients with bipolar disorder hospitalized in this hospital. The educational intervention was conducted in person and in a dedicated educational space located in the psychiatric ward of the hospital, a separate and dedicated room designated for educational and counseling activities, with proper ventilation, simple audiovisual equipment, and standard chairs for small group settings.
A total of 60 caregivers of bipolar disorder patients were selected through convenience sampling, and then were randomly assigned to the intervention (n=30) and control (n=30) groups using a simple random allocation method. The inclusion criteria were: age ≥18 years, spending the most time caring for the client, mental health, no drug or alcohol use, no visual or hearing impairment, and full consent to participate in the study for family caregivers. The exclusion criteria also included withdrawal from further cooperation in the research, educational program, and the occurrence of an unpredictable stressful event or incident for the participant.
The sample size was calculated based on the study by Heidari et al., 2015 (23) and according to the following formula with x1=56.07, s1=8.35, x2=68.80, s2=9.85, and type I error 0.05 and type II error 0.20; therefore, the sample size was estimated to be 25 people in each group, which was 50 people in total. However, considering the possibility of a 20% dropout, the sample size was increased to 30 people in each group to maintain the statistical power of the study in case of dropout. First, 60 people were selected from all the caregivers of the patient who met the inclusion criteria and then they were randomly divided into two intervention and control groups.
The data collection tool consisted of Demographic characteristics checklist, Caregiver Burden (CBI), and Connor-Davidson Resilience Scale (CD-RISC).
Demographic characteristics checklist included age, gender, marital status, education level, occupation, economic status, number of household members, number of affected individuals in the family, caregiver-client ratio, history of the client's illness, family history of the client's illness, and number of hospitalizations.
Caregiver Burden (CBI) was designed by Zarit et al. in 1985 to measure the stress experienced by caregivers of patients with physical and mental illnesses (24). The questions in this questionnaire are designed in the form of 22 items, with responses on a Likert scale including never, rarely, sometimes, most of the time and almost always with a minimum score of 0 and a maximum score of 4. The raw scores obtained by summing the scores of each individual's questionnaires ranging from 0 to 88. The severity of caregiving stress is classified into four levels: no stress (0-20), mild (21-40), moderate (41-60), and severe (61-80). Reliability of the questionnaire was assessed using the test-retest method and calculated to be 0.94 and 0.96 (25). The validity and reliability of the tool have been examined in previous studies and have acceptable content validity in all items. In the CVI dimension, the obtained scores were 0.7 to 1, which indicates the appropriateness of the items in the dimensions of simplicity, relevance, and clarity. The ICC (Intra class correlation) coefficient is 0.958 and internal consistency has been confirmed by determining the Cronbach's alpha coefficient at 0.86 (26).
Connor-Davidson Resilience Scale (CD-RISC) consists of 25 items designed by Connor and Davidson in 2003 to measure the ability to cope with threats and pressures (27). A version of the Connor-Davidson questionnaire has 10 items extracted from the 25-item questionnaire, and in the present study, the 10-item version was used to measure resilience. The questionnaire is scored in a 5-point Likert scale including not at all true (0), rarely true (1), sometimes true (2), often true (3), and completely true (4), and its range of scores is between 0 and 40. Finally, the total score obtained by each individual determines his or her level of resilience, with higher scores indicating greater resilience (27). Cronbach's alpha for this scale was 0.91, indicating good internal consistency. This scale has good validity and reliability (28). In the study by Sarijeh et al., the reliability of the resilience scale was determined by alpha coefficient, and the reliability coefficient of the scale was 0.87. Also, the results of factor analysis on this scale indicated the existence of a general factor in the scale. The KMO coefficient for this analysis was 0.89 and the Bartlett sphericity test value was 1893.83. The eigenvalue for this general factor was 6.64 (27).
Family caregivers (A family member who is primarily responsible for the care and direct follow-up of the patient with bipolar disorder after discharge to home and who lives with the patient continuously) who met the inclusion criteria were identified. After explaining the objectives of the study, ensuring confidentiality of the information, and obtaining written informed consent, these caregivers entered the study.
Convenient sampling was performed, and then participants were divided into two intervention (n=30) and control groups (n=30) using a random number table. The intervention group underwent 8 face-to-face training sessions (Two sessions per week, each session lasting 40-50 minutes) conducted by the first author [P.F.]. The training sessions were held between 10:00 AM and 12:00 PM in a dedicated room in the psychiatric ward of the hospital. The day before the first training session, the demographic information checklist, the Caregiver Stress Questionnaire, and the 10-item Connor-Davidson Resilience Scale were completed by the caregivers.
After completing four weeks of face-to-face training, telephone follow-up continued for 12 weeks. In the first month, telephone calls were made twice a week, and in the second and third months, the calls were reduced to once a week. Each telephone call lasted 20 to 25 minutes aimed to reinforce the educational material and provide individual counseling. In the case of any significant issues, the psychiatrist was informed and the caregiver was contacted again. Caregivers were also able to contact the research team daily from 8 a.m. to 8 p.m. if needed. The control group only received the usual discharge education provided in the hospital.
The post-test assessment was conducted at week 17, immediately after the end of the 16-week intervention period (4 weeks of in-person education and 12 weeks of telephone follow-up). This precise timing allowed for the measurement of the immediate and lasting effectiveness of the intervention. The training content in this study was developed based on the findings and scientific framework of the research by Rahmani et al. (2015) on the effect of psychological training for families of bipolar patients to reduce caregiving burden. This reputable Iranian study specifically addressed the training of families of bipolar patients and demonstrated the effectiveness of targeted psychological training in reducing families’ caregiving burden. The training content included topics such as recognizing symptoms of the disease, caregiving methods, stress management, and psychological support, which are fully documented and reliable from a clinical and scientific perspective (12). It is worth noting that the study by Rahmani et al., which was the basis for designing our educational content, has officially confirmed and established the face validity and content validity of psychological training by 10 faculty members of the Department of Psychiatry, Clinical Psychology, and Psychiatric Nursing at Tabriz University of Medical Sciences. This indicates the standardization, scientific accuracy, and applicability of the educational content used in our study caregivers.
The data were analyzed using SPSS software (Version 25). Independent and paired t-tests were used for intergroup and intragroup comparisons. P<0.05 was considered statistically significant.
Results
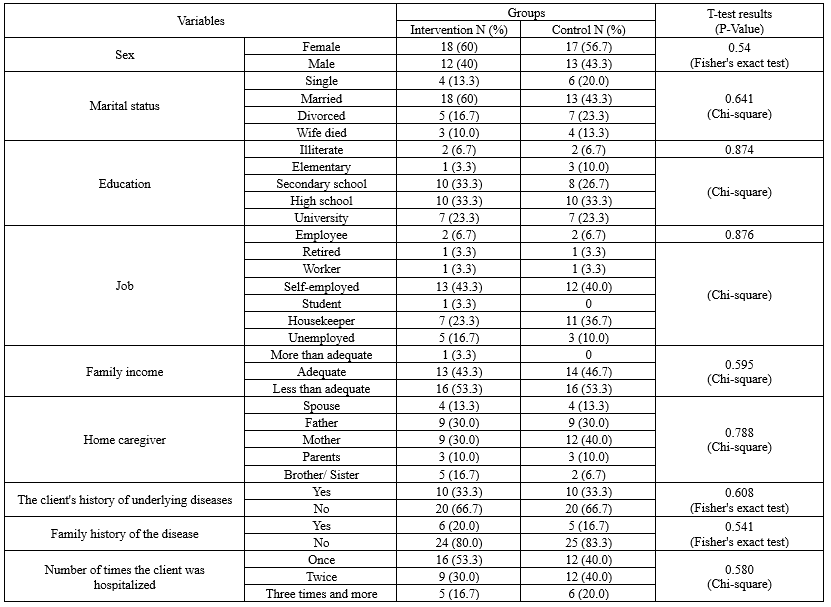
The mean age of the caregivers in the intervention and control groups were 49.90 ± 8.72 and 49.43 ± 8.69, respectively. The results of t-test did not show a significant difference in this respect (p=0.836). Other information is presented in Table 1.
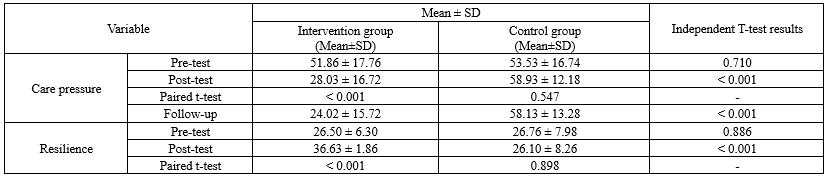
The mean of care pressure of caregivers of bipolar patients after routine care in the control group decreased from 53.53±16.74 to 58.93±12.18, and the difference was not significant (p=0.547). However, in the intervention group after telenursing, the mean of care pressure of caregivers of bipolar patients significantly decreased from 51.86±17.76 to 28.03±16.72 (p<0.0001) (Table 2). The mean of resilience of caregivers of bipolar patients after routine care in the control group decreased from 26.76±7.98 to 26.10±8.26; no significant difference was observed in this regard (p=0.898). However, in the intervention group after telenursing, mean of resilience of caregivers of bipolar patients significantly increased from 26.50±6.30 to 36.63±1.86 (p<0.0001) (Table 2). Before the intervention, there was no significant difference between the two groups in terms of care pressure and resilience (p>0.05) (Table 2).
After 16 weeks of follow-up, the mean of care pressure and resilience in the group receiving telenursing interventions had significantly increased compared to the control group (p<0.001); indicating that the telenursing intervention has lasting effects (Table 2).
Bipolar disorder (BD) is recognized as a multisystem illness affecting mood and cognitive, endocrine, autonomic, and sleep functions (1). According to the World Health Organization (WHO), there are approximately 45 million cases of bipolar disorder worldwide (2). In Iran, the prevalence of BD is 25% to 31% (3,4). Bipolar disorder has been ranked among the most disabling disorders due to its unavoidable and severe consequences, recurrent nature, and high costs. Special attention has been paid to the care and treatment of patients with this disorder and have emphasized the role of families in caring for these patients (5,6). One of the goals of the World Health Organization in promoting mental health and treating mental illnesses in recent years is to reduce the length of hospital stays and expand social services (7). More than 60% of clients who are discharged from mental disorders centers return to their families and receive their complementary care (8).
Families are the primary source of care for people with severe mental disorders. They provide financial, companionship, emotional, and health care support to members of the family with mental disorders at home. However, the development of bipolar disorder in one family member affects the entire family, causing a loss of family coping skills and strength (9). Caring for these patients depletes the family's energy and causes despair, helplessness, depression, exhaustion, and emergence or exacerbation of psychosomatic disorders in other family members, especially the primary caregivers (10). These consequences are more pronounced in individuals who have a greater role in patient’s care (11). As a result, all family members, especially the primary caregiver, experience high levels of caregiving stress, which can cause high levels of stress, depression, and low self-efficacy in caregivers (12). This care pressure depends on the factors such as age and gender of the caregivers, the quality of their previous relationship with the client, the caregivers' assessment of the situation, their perception of the illness, and the coping strategies used by the caregivers. On the other hand, caregivers by resilience can overcome the stress of caring for a client with a mental disorder and maintain their own and their family's health (13).
Resilience means controlling or acting on stressors before they harm the individual; resilient behaviors help individuals overcome negative experiences and transform them into positive ones. The characteristics of resilience include flexibility, tirelessness, self-awareness, and altruism (14). The studies have shown that coping skills training and resilience-building programs produce effective results for clients and their caregivers. Considering the role of families in the care of patients with bipolar disorder, their systematic education has been emphasized (12). Telenursing is a method used to provide remote care services at home, especially for patients who are immobile or live in remote and rural areas, and those with chronic conditions such as chronic obstructive pulmonary disease, diabetes, congenital heart disease, disability and incapacity, and chronic neurological disorders (Parkinson's and Alzheimer's) (15). Telenursing is established through video conferencing, video phone, and the Internet without time or place restrictions; it provides the possibility of educating patients and their families and providing remote consultation and sending educational programs to patients and their relatives via email (16,17).
Caring for a patient with a mental disorder imposes a lot of pressure and stress on family members, which reduces the quality of life in these individuals. Family pressures and stresses may increase the risk of relapse in the patient (18). Telenursing reduced the burden of care for healthcare staff but increased their performance (19). Abdigaravand et al. in 2023 reported the effect of education and telephone follow-up to reduce the burden of caring for families of cancer patients (20). Telephone consultations facilitate patient access, reduce costs, and eliminate time and location barriers (21). Another research indicated that telephone training has reduced the burden of care for healthcare professionals but increased their performance (22). Among all patient education methods, telenursing is a common method to support patients and nurses. It is cost-effective because it prevents readmissions and improves the quality of care. Although research studies have expanded over the past decade, there is an urgent and serious need to strengthen and expand such projects, especially in the development, design, and evaluation of effective family intervention strategies. There is also a continuing need to improve and enhance the level of psychiatric service delivery to severely mentally ill patients and their families (18). In particular, reducing the burden of care and increasing the resilience of family members in caring for a mentally ill patient are essential. Therefore, the present study was conducted with aim to evaluate the effect of education and telephone follow-up after discharge (Telenursing) on care pressure and resilience of caregivers of bipolar patients.
Methods
This quasi-experimental study with a pre-test and post-test design and a control group was conducted from September 2024 to March 2025 at Razi Psychiatric Hospital in Tehran. The statistical population consisted of family caregivers of clients with bipolar disorder hospitalized in this hospital. The educational intervention was conducted in person and in a dedicated educational space located in the psychiatric ward of the hospital, a separate and dedicated room designated for educational and counseling activities, with proper ventilation, simple audiovisual equipment, and standard chairs for small group settings.
A total of 60 caregivers of bipolar disorder patients were selected through convenience sampling, and then were randomly assigned to the intervention (n=30) and control (n=30) groups using a simple random allocation method. The inclusion criteria were: age ≥18 years, spending the most time caring for the client, mental health, no drug or alcohol use, no visual or hearing impairment, and full consent to participate in the study for family caregivers. The exclusion criteria also included withdrawal from further cooperation in the research, educational program, and the occurrence of an unpredictable stressful event or incident for the participant.
The sample size was calculated based on the study by Heidari et al., 2015 (23) and according to the following formula with x1=56.07, s1=8.35, x2=68.80, s2=9.85, and type I error 0.05 and type II error 0.20; therefore, the sample size was estimated to be 25 people in each group, which was 50 people in total. However, considering the possibility of a 20% dropout, the sample size was increased to 30 people in each group to maintain the statistical power of the study in case of dropout. First, 60 people were selected from all the caregivers of the patient who met the inclusion criteria and then they were randomly divided into two intervention and control groups.
The data collection tool consisted of Demographic characteristics checklist, Caregiver Burden (CBI), and Connor-Davidson Resilience Scale (CD-RISC).
Demographic characteristics checklist included age, gender, marital status, education level, occupation, economic status, number of household members, number of affected individuals in the family, caregiver-client ratio, history of the client's illness, family history of the client's illness, and number of hospitalizations.
Caregiver Burden (CBI) was designed by Zarit et al. in 1985 to measure the stress experienced by caregivers of patients with physical and mental illnesses (24). The questions in this questionnaire are designed in the form of 22 items, with responses on a Likert scale including never, rarely, sometimes, most of the time and almost always with a minimum score of 0 and a maximum score of 4. The raw scores obtained by summing the scores of each individual's questionnaires ranging from 0 to 88. The severity of caregiving stress is classified into four levels: no stress (0-20), mild (21-40), moderate (41-60), and severe (61-80). Reliability of the questionnaire was assessed using the test-retest method and calculated to be 0.94 and 0.96 (25). The validity and reliability of the tool have been examined in previous studies and have acceptable content validity in all items. In the CVI dimension, the obtained scores were 0.7 to 1, which indicates the appropriateness of the items in the dimensions of simplicity, relevance, and clarity. The ICC (Intra class correlation) coefficient is 0.958 and internal consistency has been confirmed by determining the Cronbach's alpha coefficient at 0.86 (26).
Connor-Davidson Resilience Scale (CD-RISC) consists of 25 items designed by Connor and Davidson in 2003 to measure the ability to cope with threats and pressures (27). A version of the Connor-Davidson questionnaire has 10 items extracted from the 25-item questionnaire, and in the present study, the 10-item version was used to measure resilience. The questionnaire is scored in a 5-point Likert scale including not at all true (0), rarely true (1), sometimes true (2), often true (3), and completely true (4), and its range of scores is between 0 and 40. Finally, the total score obtained by each individual determines his or her level of resilience, with higher scores indicating greater resilience (27). Cronbach's alpha for this scale was 0.91, indicating good internal consistency. This scale has good validity and reliability (28). In the study by Sarijeh et al., the reliability of the resilience scale was determined by alpha coefficient, and the reliability coefficient of the scale was 0.87. Also, the results of factor analysis on this scale indicated the existence of a general factor in the scale. The KMO coefficient for this analysis was 0.89 and the Bartlett sphericity test value was 1893.83. The eigenvalue for this general factor was 6.64 (27).
Family caregivers (A family member who is primarily responsible for the care and direct follow-up of the patient with bipolar disorder after discharge to home and who lives with the patient continuously) who met the inclusion criteria were identified. After explaining the objectives of the study, ensuring confidentiality of the information, and obtaining written informed consent, these caregivers entered the study.
Convenient sampling was performed, and then participants were divided into two intervention (n=30) and control groups (n=30) using a random number table. The intervention group underwent 8 face-to-face training sessions (Two sessions per week, each session lasting 40-50 minutes) conducted by the first author [P.F.]. The training sessions were held between 10:00 AM and 12:00 PM in a dedicated room in the psychiatric ward of the hospital. The day before the first training session, the demographic information checklist, the Caregiver Stress Questionnaire, and the 10-item Connor-Davidson Resilience Scale were completed by the caregivers.
After completing four weeks of face-to-face training, telephone follow-up continued for 12 weeks. In the first month, telephone calls were made twice a week, and in the second and third months, the calls were reduced to once a week. Each telephone call lasted 20 to 25 minutes aimed to reinforce the educational material and provide individual counseling. In the case of any significant issues, the psychiatrist was informed and the caregiver was contacted again. Caregivers were also able to contact the research team daily from 8 a.m. to 8 p.m. if needed. The control group only received the usual discharge education provided in the hospital.
The post-test assessment was conducted at week 17, immediately after the end of the 16-week intervention period (4 weeks of in-person education and 12 weeks of telephone follow-up). This precise timing allowed for the measurement of the immediate and lasting effectiveness of the intervention. The training content in this study was developed based on the findings and scientific framework of the research by Rahmani et al. (2015) on the effect of psychological training for families of bipolar patients to reduce caregiving burden. This reputable Iranian study specifically addressed the training of families of bipolar patients and demonstrated the effectiveness of targeted psychological training in reducing families’ caregiving burden. The training content included topics such as recognizing symptoms of the disease, caregiving methods, stress management, and psychological support, which are fully documented and reliable from a clinical and scientific perspective (12). It is worth noting that the study by Rahmani et al., which was the basis for designing our educational content, has officially confirmed and established the face validity and content validity of psychological training by 10 faculty members of the Department of Psychiatry, Clinical Psychology, and Psychiatric Nursing at Tabriz University of Medical Sciences. This indicates the standardization, scientific accuracy, and applicability of the educational content used in our study caregivers.
The data were analyzed using SPSS software (Version 25). Independent and paired t-tests were used for intergroup and intragroup comparisons. P<0.05 was considered statistically significant.
Results
The mean age of the caregivers in the intervention and control groups were 49.90 ± 8.72 and 49.43 ± 8.69, respectively. The results of t-test did not show a significant difference in this respect (p=0.836). Other information is presented in Table 1.
The mean of care pressure of caregivers of bipolar patients after routine care in the control group decreased from 53.53±16.74 to 58.93±12.18, and the difference was not significant (p=0.547). However, in the intervention group after telenursing, the mean of care pressure of caregivers of bipolar patients significantly decreased from 51.86±17.76 to 28.03±16.72 (p<0.0001) (Table 2). The mean of resilience of caregivers of bipolar patients after routine care in the control group decreased from 26.76±7.98 to 26.10±8.26; no significant difference was observed in this regard (p=0.898). However, in the intervention group after telenursing, mean of resilience of caregivers of bipolar patients significantly increased from 26.50±6.30 to 36.63±1.86 (p<0.0001) (Table 2). Before the intervention, there was no significant difference between the two groups in terms of care pressure and resilience (p>0.05) (Table 2).
After 16 weeks of follow-up, the mean of care pressure and resilience in the group receiving telenursing interventions had significantly increased compared to the control group (p<0.001); indicating that the telenursing intervention has lasting effects (Table 2).
|
Table 1. Comparison of demographic variables of family caregivers of bipolar disorder patients in the intervention and control groups
 |
|
Table 2. Mean of care pressure and resilience of caregivers of bipolar patients in the intervention control and groups
 |
Discussion
The result of the present study showed that the telenursing intervention has an effect on the care pressure and resilience of caregivers of bipolar patients. In line with the results of the present study, different studies have shown the effectiveness of telenursing in decreasing the care pressure of family caregivers of patients with diagnoses of hemodialysis (29), stroke (30), heart failure (31), Alzheimer’s disease, dementia (14), and Covid-19 (32). A study examining the effect of psychological training on the resilience of family caregivers of clients with bipolar disorder showed that psychological training is effective on resilience (12). Another study examined the psychological stress of family caregivers of hospitalized schizophrenia patients. Their findings showed that 12.2% of caregivers had mild, 36.4% had moderate, and 51.4% had severe psychological stress (33). In the present study, caregivers also endured high caregiving stress. Care pressure in the families of patients with bipolar affective disorder was investigated in the other study, which indicated that greater care pressure was associated with longer duration of illness and more life cycles, and care pressure was high in the families of patients with bipolar disorder (34). Care pressure has been reported as a predictor of depression among family and friends caring for people with bipolar disorder (35). In a cross-sectional study, fifty-one patients with bipolar disorder who were attending an outpatient clinic were evaluated. Care pressure among their caregivers was assessed using the Care pressure Assessment Schedule and it was found that caregivers experienced higher care pressure (36).
Telenursing is the use of information and communication technologies to develop all fields of nursing care, education and research at a distance (37). Telenursing is utilized to improve nursing care processes and competencies, lessen time and location-based disparities in nursing care access, and support nursing education, training, and scientific advancement. Since telenursing saves nursing time and resources, allows nurses to provide care, monitoring, and education, wherever and whenever needed, and gives consumers information to encourage self-care (16).
Traditional services are provided by the healthcare system in Iran. Although all complications from traditional methods cannot currently be managed by telenursing, but factors such as access to care, cost-effective delivery and the distribution of scarce providers are well addressed by telenursing. The development of telenursing techniques is actually an attempt to get around the geographical and temporal barriers to care service delivery. Patients receive the care they require as soon as possible, which allow for good spatial control. The chronic nature of heart failure and the need to provide these patients with faster care services make telenursing systems necessary. Patients with heart failure make up a significant percentage of chronic patients (31).
The strengths of the present study include the random selection of the study population and the use of control groups, which was also provided with an educational brochure produced following completion of the study that was a useful guide for caregivers. One of the study's limitations was receiving training and information from other sources that could affected the study's findings, which were partially managed by using a control group. Furthermore, people differed in their capacity to handle crises and issues as well as adjust to them, which may have an effect on unsustainable results.
Conclusion
As evidenced by the results of the present study, education and telephone follow-up after discharge (Telenursing) was positively effective on care pressure and resilience of caregivers of bipolar patients. These results can be used to educate caregivers in different diseases. To confirm and verify the present results, future studies with longer intervention duration should be conducted. Considering the effect of telenursing on reducing caregiver pressure and increasing resilience in caregivers of bipolar patients, this method can also be considered as an auxiliary method for controlling the symptoms.
Acknowledgement
The authors would like to express their gratitude to the respected authorities and families of the patients who participated in this study.
Funding sources
The authors received no financial support for the research, authorship, and/or publication of this article
Ethical statement
This research was approved by the Committee of Ethics in Human Research at Neyshabur University of Medical Sciences (Ethical code: IR.NUMS.REC.1403.059). All participants signed informed written consent after the relevant procedures and the purpose of the study were fully explained. Also, all patients completed all questionnaires. All participants first filled out an informed consent form and then entered the study. All methods were carried out in accordance with the Declaration of Helsinki. All participants’ information was preserved and they had the right to withdraw from the study.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All authors participated in the design and formulation of the study. PF was involved in data collection. AKh prepared the initial draft of the article. PF, AKh, and MF carefully reviewed and revised the research design, data analysis, and interpretation of results. SS participated in the review of the final version of the article. All statistical analyses were performed by the research team and there was no separate statistical consultant involved in this study. All authors read and approved the final version of the article.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Type of study: Original Article |
Subject:
Nursing
References
1. Ahmad S. Kaplan Sadock's Pocket Handbook of Clinical Psychiatry: Lippincott Williams & Wilkins. 2024. [View at Publisher] [Google scholar]
2. Nierenberg AA, Harris MG, Kazdin AE, Puac‐Polanco V, Sampson N, Vigo DV, et al. Perceived helpfulness of bipolar disorder treatment: findings from the World Health Organization World Mental Health Surveys. Bipolar disorders. 2021;23(6):565-83. [View at Publisher] [DOI] [PMID] [Google scholar]
3. Badrfam R, Zandifar A, Sadighi Gilani M, Rouhbakhsh A, Farid M, Faraji S, et al. Prevalence of psychosis and its relationship with substance use disorder in patients with bipolar disorder in Iran. J Affect Disord Rep. 2024;16:100778. [View at Publisher] [DOI] [Google Scholar]
4. Shaker Z, Goudarzi Z, Ravangard R, Shaker Z, Hedayati A, Keshavarz K. The economic burden of bipolar disorder: a case study in Southern Iran.Cost Eff Resour Alloc. 2024;22(1):55. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Primers . 2018;4(1):1-16. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Franchini L, Barbini B, Zanardi R, Fregna L, Martini F, Manfredi E, et al. Mood disorders. In Fundamentals of Psychiatry for Health Care Professionals 2022;(pp. 49-84). [View at Publisher] [DOI] [Google Scholar]
7. Goes FS. Diagnosis and management of bipolar disorders. BMJ. 2023P;381:e073591. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Lohrasbi F, Alavi M, Akbari M, Maghsoudi J. Promoting psychosocial health of family caregivers of patients with chronic mental disorders: A review of challenges and strategies. Chonnam Med J. 2023;59(1):31-47. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Shamsaei F, Mohammadkhan Kermanshahi S, Vanaki Z. Survey of family caregiver needs of patients with bipolar disorder. Avicenna Journal of Clinical Medicine. 2010;17(3):57-63. [View at Publisher] [Google Scholar]
10. Pickett-Schenk SA, Cook JA, Laris A. Journey of Hope program outcomes. Community Ment Health J. 2000;36(4):413-24. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Pattyn N, Hauffa R. Handbook of Mental Performance: Taylor & Francis; 2024. [View at Publisher] [DOI] [Google Scholar]
12. Rahmani F, Ebrahimi H, Ranjbar F, Asghari E. The effect of group psychoeducational program on attitude toward mental illness in family caregivers of patients with bipolar disorder. Hayat. 2016;21(4):65-79 [View at Publisher] [Google Scholar]
13. Sari A, Duman ZÇ. Effects of the family support and psychoeducation program based on the Calgary Family Intervention Model on the coping, psychological distress and psychological resilience levels of the family caregivers of chronic psychiatric patients. Arch Psychiatr Nurs. 2022;41:1-10. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Sadeghmoghadam L, Shahriyan F, Delshad A, Deluee MA. The effect of educational intervention by tele‐nursing on caregiver burden in family caregivers of elderly with Alzheimer's disease: dementia care research: dementia care‐models of care. Alzheimers Dement. 2020;16(57):e040961. [View at Publisher] [DOI] [Google Scholar]
15. Safa A, Saberi F, Sabery M, Mirbagher Ajorpaz N. Effect of Telephone Counseling on Self-Efficacy in Self-Care Behaviors of Patients with COVID-19. J Res Dev Nurs Midw 2022;19(1):25-9 [View at Publisher] [DOI] [Google Scholar]
16. Gu D, Dupre ME, Klimczuk A, Magdalena Klimczuk-Kochańska M. Encyclopedia of Gerontology and Population Aging. Springer. 2021.4952-6 [View at Publisher] [DOI] [Google Scholar]
17. Mojarad Kahani A, Ghanbari Hashem Abadi BA, Soltanian Gh. The efficacy of group psycho educational interventions on level of depression, anxiety and burden experienced (stress) in families of patients with bipolar disorders. RBS. 2015;13(3):420-30. [View at Publisher] [Google Scholar]
18. Cham CQ, Ibrahim N, Siau CS, Kalaman CR, Ho MC, Yahya AN, et al. Caregiver burden among caregivers of patients with mental illness: A systematic review and meta-analysis. Healthcare (Basel). 2022;10(12):2423. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Chiang L-C, Chen W-C, Dai Y-T, Ho Y-L. The effectiveness of telehealth care on caregiver burden, mastery of stress, and family function among family caregivers of heart failure patients: a quasi-experimental study. Int J Nurs Stud. 2012;49(10):1230-42. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Abdigaravand M, Goudarzi F, Hasanvand S, Birjandi M, Galehdar N, Hojati Z. The effect of education and telephone follow-up on the burden of family caregivers of patients with cancer. SAGE Open Nurs. 2023;9:23779608231170444. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Liptrott S, Bee P, Lovell K. Acceptability of telephone support as perceived by patients with cancer: a systematic review. Eur J Cancer Care (Engl). 2018;27(1):e12643. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Ghorbani F, Zare M, Heshmati Nabavi F, Behnam Vashani H, Bari A. Effect of education and telephone counseling on caregiver strain and unmet needs in family caregivers and self-care behaviors in patients with cancer: a randomized clinical trial. Evidence Based Care. 2020;10(1):51-60. [View at Publisher] [DOI] [Google Scholar]
23. Heidari M, Fayazi S, Borsi H, Moradbeigi K, Akbari Nassaji N. Effect of a self-management program based on 5A model on dyspnea and fatigue severity among patients with chronic obstructive pulmonary disease: a randomized clinical trial. Hayat. 2015;20(4):89-9. [View at Publisher] [Google Scholar]
24. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649-55. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Shafiezadeh A, Heravi-Karimoo M, Rejeh N, Sharif Nia H, Montazeri A. Translation and primarily validation of the Persian Version of Caregiver Burden Inventory. Payesh (Health Monitor). 2019;18(4):405-14. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Raesi R, Mirzaei A, Saghari S, Raei M, Bokaie S, Hushmandi K. Investigating the Effect of Tele-Nursing on the Care Burden of Family Caregivers of COVID- 19 Patients. J Crit Care Nurs. 2021;14(3):21-9 [View at Publisher] [DOI] [Google Scholar]
27. sarijeh PF, Kia B, Mahmoodi M, Salahi Nejad M. The Effect of Spiritual Therapy on Resiliency of Hemodialysis Patients. Avicenna J Nurs Midwifery Care. 2021;29(4):264-72 [View at Publisher] [DOI] [Google Scholar]
28. fereidouni sarijeh P, khatib A. The relationship between believing in resurrection and resilience and feeling of social and emotional loneliness. Evidence Based Care. 2025;15(2):47-54. [View at Publisher] [DOI] [Google Scholar]
29. Ghane G, Farahani MA, Seyedfatemi N, Haghani H. Effectiveness of supportive educative program on the burden in family caregivers of hemodialysis patients. Nursing And Midwifery Journal. 2017;14(10):885-95. [View at Publisher] [Google Scholar]
30. Goudarzian M, Fallahi-Khoshknab M, Dalvandi A, Delbari A, Biglarian A. Effect of telenursing on levels of depression and anxiety in caregivers of patients with stroke: A randomized clinical trial. Iran J Nurs Midwifery Res. 2018;23(4):248-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
31. Namjoo M, Nematollahi M, Taebi M, Kahnooji M, Mehdipour-Rabori R. The efficacy of telenursing on caregiver burden among Iranian patients with heart failure: A randomized clinical trial. ARYA Atheroscler. 2021;17(6):1-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Rad M, Rajab Dizavandi F, Rajab Dizavandi A. The Effect of Education through Telenursing on the Caregiver Burden among Family Caregivers of COVID‐19 Patients: A Randomized Clinical Trial. Perspect Psychiatr Care. 2023;2023(1):2545639. [View at Publisher] [DOI] [Google Scholar]
33. Haresabadi M, Bibak B, HOSEIN ZE, Bayati M, Arki M, Akbari H. Assessing burden of family caregivers of patients with schizophrenia admitted in Imam Reza Hospital-Bojnurd 2010. Journal of North Khorasan University of Medical Sciences .2012;4(2):165-71 [View at Publisher] [DOI] [Google Scholar]
34. Gania AM, Kaur H, Grover S, Khan A, Suhaff A, Baidya K, et al. Caregiver burden in the families of the patients suffering from bipolar affective disorder. BJMP. 2019;12(1):a006. [View at Publisher] [Google Scholar]
35. Perlick DA, Berk L, Kaczynski R, Gonzalez J, Link B, Dixon L, et al. Caregiver burden as a predictor of depression among family and friends who provide care for persons with bipolar disorder. Bipolar disorders. 2016;18(2):183-91. [View at Publisher] [DOI] [PMID] [Google Scholar]
36. Vasudeva S, Sekhar CK, Rao PG. Caregivers burden of patients with schizophrenia and bipolar disorder: a sectional study.Indian J Psychol Med. 2013;35(4):352-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
37. Abdallah ZA, Khamis EAR, Ibrahim FM, Farag AAW. Telenursing Future in Solving the Nursing Global Workforce Gap. Nursing-Trends and Developments: IntechOpen. 2024. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |