Volume 20, Issue 2 (10-2023)
J Res Dev Nurs Midw 2023, 20(2): 30-33 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghaderi R, Mahmoodi-Shan G R, Taziki M H, Behnampour N. Association between satisfaction with hearing aid use and quality of life among elderly individuals with hearing loss. J Res Dev Nurs Midw 2023; 20 (2) :30-33
URL: http://nmj.goums.ac.ir/article-1-1289-en.html
URL: http://nmj.goums.ac.ir/article-1-1289-en.html
1- Geriatric Nursing student, Nursing and Midwifery Faculty, Golestan University of Medical Sciences, Gorgan, Iran
2- Nursing Research Center, Nursing and Midwifery Faculty, Golestan University of Medical Sciences, Gorgan, Iran ,Mahmoodigh@yahoo.com
3- Department of Surgery, School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran
2- Nursing Research Center, Nursing and Midwifery Faculty, Golestan University of Medical Sciences, Gorgan, Iran ,
3- Department of Surgery, School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran
Full-Text [PDF 430 kb]
(1059 Downloads)
| Abstract (HTML) (3005 Views)
Full-Text: (746 Views)
Introduction
Hearing loss is considered one of the most common chronic diseases and the second most debilitating among the elderly. Approximately one-third of those over 65 have hearing loss (1). The prevalence of hearing loss doubles in the seventh decade (60 to 69 years of age) (1). Hearing loss is defined as over 40 dB in adults and more than 30 dB in children. Hearing loss can take different forms, such as sensorineural, transient, and mixed (2). Regarding intensity, hearing loss is categorized as mild, with a hearing threshold of 26 - 40 dB; moderate, 41 - 65 dB; severe, 66 - 90 dB; and profound, 91 dB or higher (3). A study on age-related hearing loss in Korea indicated that the prevalence of unilateral hearing loss was 8%, and bilateral hearing loss was 5.9%. Men were 53.4% more likely to have hearing loss than women (4).
Hearing loss can lead to problems such as disrupted interpersonal relationships, restricted participation in social activities, dependence on family support, isolation, depression, and cognitive dysfunction in the elderly (4). It can also create adverse physiological, social, and occupational outcomes in their daily lives (5). Utilizing rehabilitation programs and hearing-assisting devices such as hearing aids can help older individuals return to everyday life, positively impacting their quality of life and satisfaction and their families (7). Despite these positive effects, using a hearing aid is accompanied by some inconveniences, including cost, device setup disruptions, extra noise in the ear, installation and maintenance difficulties, frequent battery replacement, hearing aid failures, and medical costs. These factors have caused the elderly to be reluctant to acquire and use hearing-assisting devices, which can affect their quality of life and satisfaction with using the device over time (6, 7).
Satisfaction is a significant outcome in medical care, and determining its level is an essential criterion for measuring the quality of medical health and rehabilitation services (8). Satisfaction with rehabilitation devices depends on the device's function and the users' attitude (7). A study indicated that rehabilitation programs, particularly hearing aid use, have positively impacted the quality of life of hearing loss individuals. Quality of life is considered a part of health and a primary indicator in individuals' lives, used when evaluating medical health programs (9, 10). The major challenge for the elderly with hearing loss is the change in their quality of life, satisfaction, and continued use of hearing-assisting devices (11). Recent studies have indicated that the participation and cooperation of various organizations in meeting the needs of the elderly and promoting their quality of life are necessary (12). The Health Insurance Office is a center that provides hearing aid devices for the elderly. It is necessary to acquire the required knowledge about hearing aid users' satisfaction among the elderly. Therefore, the study was conducted to determine the association between hearing aid use satisfaction and the quality of life among elderly individuals with hearing loss.
Methods
The study is cross-sectional research conducted on elderly individuals with hearing loss who were fitted with Hearing Aids (HAs). The samples were selected from elderly individuals who had received HAs from the Health Insurance Office in Gorgan, Iran. There were 186 cases, of which 60 subjects who met the inclusion criteria were conveniently selected. The study was conducted from May to October 2019.
The inclusion criteria included elderly individuals over 60 years of age suffering from hearing loss and fitted with HAs, per the audiometry protocol for hearing loss. Additionally, the criteria required that the individuals had been using HAs for more than 6 weeks and had no recognized psychiatric disorders, psychosis, Alzheimer's disease, or dementia.
According to Khayavi et al.'s study, which compared senior citizens' satisfaction with HAs based on hearing loss type and level, the sample size was estimated at 42 with α=0.05 and β=0.1. Considering a 25% sample loss, the final sample size was 52 subjects (13). The sampling was conducted randomly among eligible elderly individuals by the lists of records maintained by the Health Insurance Office for the Elderly.
Data collection was performed through personal interviews at the residences of the elderly individuals. The demographic information collected included age, gender, marital status, education, job status, individual's perception of economic status, hearing loss duration, daily usage level, and HA usage duration. HA use satisfaction data were gathered using the "Satisfaction with Amplification in Daily Life" (SADL) questionnaire and The Short Form Health Survey of Quality of Life (SF-12).
The SADL scale comprised 15 items with 4 subscales, including:
Hearing loss is considered one of the most common chronic diseases and the second most debilitating among the elderly. Approximately one-third of those over 65 have hearing loss (1). The prevalence of hearing loss doubles in the seventh decade (60 to 69 years of age) (1). Hearing loss is defined as over 40 dB in adults and more than 30 dB in children. Hearing loss can take different forms, such as sensorineural, transient, and mixed (2). Regarding intensity, hearing loss is categorized as mild, with a hearing threshold of 26 - 40 dB; moderate, 41 - 65 dB; severe, 66 - 90 dB; and profound, 91 dB or higher (3). A study on age-related hearing loss in Korea indicated that the prevalence of unilateral hearing loss was 8%, and bilateral hearing loss was 5.9%. Men were 53.4% more likely to have hearing loss than women (4).
Hearing loss can lead to problems such as disrupted interpersonal relationships, restricted participation in social activities, dependence on family support, isolation, depression, and cognitive dysfunction in the elderly (4). It can also create adverse physiological, social, and occupational outcomes in their daily lives (5). Utilizing rehabilitation programs and hearing-assisting devices such as hearing aids can help older individuals return to everyday life, positively impacting their quality of life and satisfaction and their families (7). Despite these positive effects, using a hearing aid is accompanied by some inconveniences, including cost, device setup disruptions, extra noise in the ear, installation and maintenance difficulties, frequent battery replacement, hearing aid failures, and medical costs. These factors have caused the elderly to be reluctant to acquire and use hearing-assisting devices, which can affect their quality of life and satisfaction with using the device over time (6, 7).
Satisfaction is a significant outcome in medical care, and determining its level is an essential criterion for measuring the quality of medical health and rehabilitation services (8). Satisfaction with rehabilitation devices depends on the device's function and the users' attitude (7). A study indicated that rehabilitation programs, particularly hearing aid use, have positively impacted the quality of life of hearing loss individuals. Quality of life is considered a part of health and a primary indicator in individuals' lives, used when evaluating medical health programs (9, 10). The major challenge for the elderly with hearing loss is the change in their quality of life, satisfaction, and continued use of hearing-assisting devices (11). Recent studies have indicated that the participation and cooperation of various organizations in meeting the needs of the elderly and promoting their quality of life are necessary (12). The Health Insurance Office is a center that provides hearing aid devices for the elderly. It is necessary to acquire the required knowledge about hearing aid users' satisfaction among the elderly. Therefore, the study was conducted to determine the association between hearing aid use satisfaction and the quality of life among elderly individuals with hearing loss.
Methods
The study is cross-sectional research conducted on elderly individuals with hearing loss who were fitted with Hearing Aids (HAs). The samples were selected from elderly individuals who had received HAs from the Health Insurance Office in Gorgan, Iran. There were 186 cases, of which 60 subjects who met the inclusion criteria were conveniently selected. The study was conducted from May to October 2019.
The inclusion criteria included elderly individuals over 60 years of age suffering from hearing loss and fitted with HAs, per the audiometry protocol for hearing loss. Additionally, the criteria required that the individuals had been using HAs for more than 6 weeks and had no recognized psychiatric disorders, psychosis, Alzheimer's disease, or dementia.
According to Khayavi et al.'s study, which compared senior citizens' satisfaction with HAs based on hearing loss type and level, the sample size was estimated at 42 with α=0.05 and β=0.1. Considering a 25% sample loss, the final sample size was 52 subjects (13). The sampling was conducted randomly among eligible elderly individuals by the lists of records maintained by the Health Insurance Office for the Elderly.
Data collection was performed through personal interviews at the residences of the elderly individuals. The demographic information collected included age, gender, marital status, education, job status, individual's perception of economic status, hearing loss duration, daily usage level, and HA usage duration. HA use satisfaction data were gathered using the "Satisfaction with Amplification in Daily Life" (SADL) questionnaire and The Short Form Health Survey of Quality of Life (SF-12).
The SADL scale comprised 15 items with 4 subscales, including:
- Positive effects of communication with others
- Evaluation of cost and services related to audiologist competency and hearing aid devices
- Analysis of negative features related to use in noisy places and phone use
- Measurement of self-concept, reflecting the user's mental image and feelings
Participants responded using a 7-option Likert scale, ranging from "absolutely agree" to "disagree." Scores ranged from 15 to 105, with scores below 20 indicating very dissatisfied, scores from 20 to 80 indicating dissatisfied, and scores higher than 80 indicating very satisfied. The original survey was validated in 2001 by the designers (13, 14). Content validity was measured , and reliability was found to be 0.80 (15).
The SF-12 assesses individuals' general perception of their health, including physical function, bodily health, emotional well-being, physical pain, social function, joy, vital energy, and psychological health. Responses are on a 5-option Likert scale. The overall score ranges from 12 to 48, categorized into three classes: poor (12-24), mild (25-36), and good quality of life (37-48). This scale has been validated in the elderly community and the broader Iranian society, with its validity and reliability confirmed through test-retest analysis (r=0.9) (14).
Data analysis was performed using SPSS-18. The Chi-squared test determined the relationship between qualitative variables, the independent T-test compared two groups, and the Mann-Whitney U test was used for variables with non-normal distributions. ANOVA, the Kruskal-Wallis test, and the Spearman correlation coefficient were employed to assess relationships between variables. The level of significance was set at P < 0.05.
Results
In this study, 60 elderly individuals with hearing loss over 60 participated, with a mean age of 76.85±8.16. Most participants were male, had limited formal education, were married, homemakers, or retired.
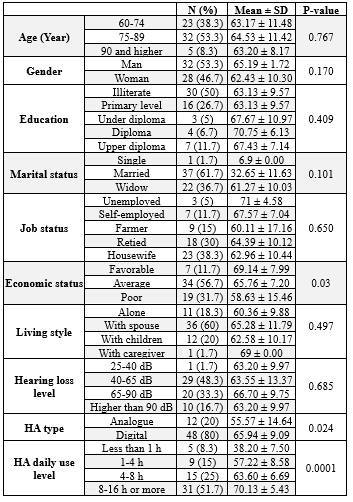
Regarding economic status, a significant portion (56.7%) reported an average economic status, while 60% lived with their spouses and only 1.7% lived with caregivers. Notably, 90% of the elderly reported the onset of hearing loss occurring at or after the age of 55. Sensorineural hearing loss was the predominant type (71.7 %), and most (48.3 %) experienced hearing loss in the 40 to 65 dB range. Additionally, 80% were equipped with digital HA, with 51.7% of the elderly using HAs for 8-16 hours daily (Table 1).
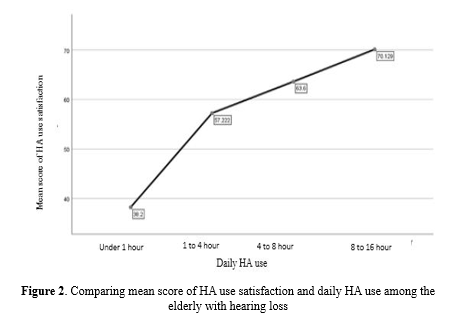
The overall mean satisfaction score with HA use was 63.90±11.074. Both the Kruskal-Wallis test and ANOVA revealed a significant association between mean HA use satisfaction scores and the elderly's economic status (P=0.03), HA type (P=0.024), and daily HA use duration (P=0.0001) (see Table 1).
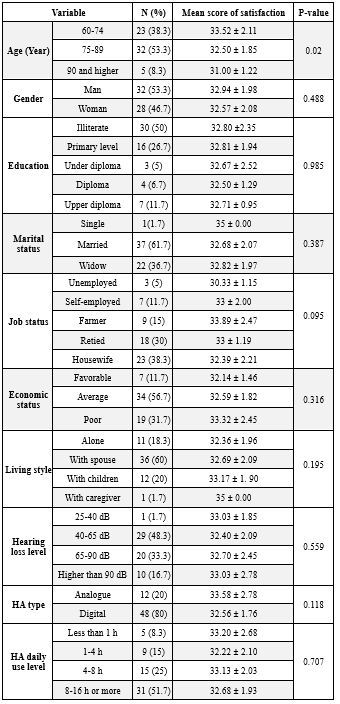
The results indicated that the mean quality of life score for elderly individuals fitted with HAs was 32.77±2.02. ANOVA tests demonstrated a significant correlation between quality-of-life scores and age groups (P=0.02), while no significant relationships were observed with other demographic variables. The mean quality of life score for those aged 40-65 dB hearing loss was 33.03±1.85, although this relationship did not reach statistical significance (P=0.559). Additionally, ANOVA tests showed no significant link between mean quality of life scores and daily HA usage among the elderly, whether using HAs for 1-4 hours daily (32.22, the lowest) or 4-8 hours daily (33.13, the highest) (Table 2).
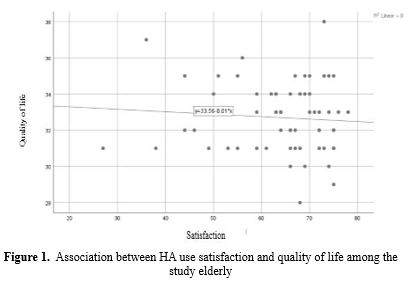
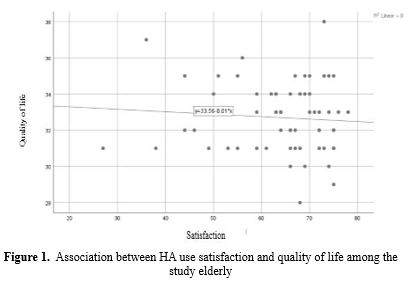
Quality of life for the elderly and HA use satisfaction exhibited an inverse but weak relationship, approximating a linear model with a negative coefficient close to zero. The Spearman correlation coefficient between HA use satisfaction and quality of life was -0.068 (P=0.511), suggesting that other factors may influence quality of life (Figure 1).
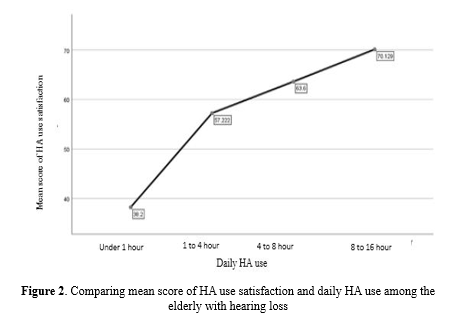
Furthermore, the results suggested that more significant HA usage throughout the day correlated with higher satisfaction mean scores (Figure 2).
Discussion
The study revealed an inverse, albeit fragile, relationship between the quality of life of elderly individuals and their satisfaction with HA usage. The Spearman correlation coefficient between HA satisfaction and quality of life was insignificant. This outcome diverged from the findings of McPherson and Kateifidis et al., who reported a significant Pearson correlation coefficient between quality of life dimensions and HA benefits (16, 17). However, it aligned with another study which reported a Pearson correlation coefficient between satisfaction and factors such as age, duration of HA use, and level of hearing loss (2). This inconsistency could be attributed to the influence of other variables on quality of life.
Despite the geographical and cultural differences between the present study and research which conducted in Brazil, there appears to be some concurrence, possibly due to similarities in the tools used and the age demographics in both studies. Notably, the average HA satisfaction score among elderly individuals with hearing loss was favorable (within the score range of 20-80), consistent with the findings of Kozlowski et al. and Faraji Khayavi et al. (1, 13).
The study uncovered a statistically significant relationship between HA satisfaction and demographic factors, including economic status, type of HA used, and daily HA usage. Elderly individuals with a favorable economic status reported a mean HA satisfaction score, indicating higher satisfaction levels. This finding suggests that individuals with higher economic status, the elderly, or their families tend to experience greater satisfaction with their hearing aids (HAs). Among the elderly participants, 80% used digital hearing aids, and their mean satisfaction with these devices was notably high. This high satisfaction can be attributed to several advantages of digital HAs, including their ability to adapt to various conditions and environments, tailor audio settings to individual needs, reduce wind-induced whistling sounds, maintain a smaller and lighter form factor compared to analog HAs, and automatically adjust ambient sounds to optimize audio quality. The duration of daily HA use showed a significant statistical relationship with HA satisfaction, with individuals using HAs for 8-16 hours reporting high satisfaction. This finding is consistent with the results of previous studies by Romanet et al. (2018), McPherson (2018), and Dashti et al., all of whom reported higher satisfaction scores among individuals using their HAs for more than 4 hours (15, 16, 18).
The present study indicated that hearing assistive devices contribute to an enhanced quality of life among the elderly. The mean quality of life score for elderly individuals in this study was relatively high, consistent with the findings of a study which indicated increased use of hearing assistive devices positively affects physical health and overall quality of life (17).
The results further demonstrated that among the demographic variables, age and quality of life in elderly individuals with hearing loss exhibited a significant statistical association. The mean quality of life score was highest in ages 60-74, with scores declining as individuals grew older. This observation corresponds with the findings of Kateifidis et al. (2017) (17), who reported a Pearson correlation coefficient of -0.43 between age and quality of life. According to research from other countries, hearing loss has been associated with increased dependence and more significant caregiving needs in the elderly, ultimately diminishing their quality of life.
Regarding education levels, the mean HA satisfaction score indicated that as education levels rise among the elderly, HA satisfaction tends to increase. However, there was a slight decrease in satisfaction in the group with higher diploma education, possibly due to other influencing factors and differing expectations regarding satisfaction. Nevertheless, this association did not reach statistical significance. The mean HA satisfaction score among married elderly individuals suggested they were more fulfilled in their daily lives and social activities. Nonetheless, this relationship was not statistically significant.
The number of background diseases in elderly individuals showed a statistically significant relationship with quality of life. As the number of background diseases increased, the mean quality of life score decreased. This research highlighted that a background disease, coupled with hearing loss, can significantly impact the quality of life of elderly individuals. Elderly individuals with hearing loss often require support from their family members. Diseases such as diabetes, cardiovascular disease, and stroke intensify this need, requiring caregivers to be more involved in the elderly individuals' daily activities and increasing their dependence. However, hearing assistive devices can substantially reduce this dependence and improve the quality of life. These findings are consistent with the studies conducted by Romanet et al. and Hussenoeder et al. (18, 19).
Conclusion
In the present study, no tangible relationship was observed between satisfaction with hearing aid use and the mean score of quality of life. However, utilizing hearing-assisting devices, such as hearing aids, has enhanced satisfaction and improved the quality of life among the elderly. As a result, increased engagement in daily activities can enhance their quality of life. Therefore, it is recommended to provide elderly individuals with education on the proper use of hearing aids to improve their quality of life further.
Acknowledgement
This manuscript is based on a master's thesis on elderly nursing approved by the Faculty of Nursing and Midwifery and the Nursing Research Center at Golestan University of Medical Sciences. We sincerely appreciate all the officials and staff of Gorgan Health Insurance and the elderly individuals who assisted us in conducting this study.
Funding sources
This study received financial support from Golestan University of Medical Sciences, Iran.
Ethical statement
The current research received approval from the Ethics Committee of Golestan University of Medical Sciences (Code IR.GUOMS.REC.1398.028). All ethical considerations were diligently observed, such as obtaining a permission letter from the Golestan Health Insurance Office, securing informed written consent and ensuring anonymity.
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Author contributions
All authors contributed to the study design and manuscript preparation; data collection was only performed by the first author and data analysis was performed by the fourth author.
The SF-12 assesses individuals' general perception of their health, including physical function, bodily health, emotional well-being, physical pain, social function, joy, vital energy, and psychological health. Responses are on a 5-option Likert scale. The overall score ranges from 12 to 48, categorized into three classes: poor (12-24), mild (25-36), and good quality of life (37-48). This scale has been validated in the elderly community and the broader Iranian society, with its validity and reliability confirmed through test-retest analysis (r=0.9) (14).
Data analysis was performed using SPSS-18. The Chi-squared test determined the relationship between qualitative variables, the independent T-test compared two groups, and the Mann-Whitney U test was used for variables with non-normal distributions. ANOVA, the Kruskal-Wallis test, and the Spearman correlation coefficient were employed to assess relationships between variables. The level of significance was set at P < 0.05.
Results
In this study, 60 elderly individuals with hearing loss over 60 participated, with a mean age of 76.85±8.16. Most participants were male, had limited formal education, were married, homemakers, or retired.
Regarding economic status, a significant portion (56.7%) reported an average economic status, while 60% lived with their spouses and only 1.7% lived with caregivers. Notably, 90% of the elderly reported the onset of hearing loss occurring at or after the age of 55. Sensorineural hearing loss was the predominant type (71.7 %), and most (48.3 %) experienced hearing loss in the 40 to 65 dB range. Additionally, 80% were equipped with digital HA, with 51.7% of the elderly using HAs for 8-16 hours daily (Table 1).
|
Table 1. Frequency and mean scores of HA usage satisfaction among elderly individuals with hearing loss
 |
The results indicated that the mean quality of life score for elderly individuals fitted with HAs was 32.77±2.02. ANOVA tests demonstrated a significant correlation between quality-of-life scores and age groups (P=0.02), while no significant relationships were observed with other demographic variables. The mean quality of life score for those aged 40-65 dB hearing loss was 33.03±1.85, although this relationship did not reach statistical significance (P=0.559). Additionally, ANOVA tests showed no significant link between mean quality of life scores and daily HA usage among the elderly, whether using HAs for 1-4 hours daily (32.22, the lowest) or 4-8 hours daily (33.13, the highest) (Table 2).
|
Table 2. Mean scores of quality of life and demographics characteristics of hearing loss suffering elderly
 |
Furthermore, the results suggested that more significant HA usage throughout the day correlated with higher satisfaction mean scores (Figure 2).
Discussion
The study revealed an inverse, albeit fragile, relationship between the quality of life of elderly individuals and their satisfaction with HA usage. The Spearman correlation coefficient between HA satisfaction and quality of life was insignificant. This outcome diverged from the findings of McPherson and Kateifidis et al., who reported a significant Pearson correlation coefficient between quality of life dimensions and HA benefits (16, 17). However, it aligned with another study which reported a Pearson correlation coefficient between satisfaction and factors such as age, duration of HA use, and level of hearing loss (2). This inconsistency could be attributed to the influence of other variables on quality of life.
Despite the geographical and cultural differences between the present study and research which conducted in Brazil, there appears to be some concurrence, possibly due to similarities in the tools used and the age demographics in both studies. Notably, the average HA satisfaction score among elderly individuals with hearing loss was favorable (within the score range of 20-80), consistent with the findings of Kozlowski et al. and Faraji Khayavi et al. (1, 13).
The study uncovered a statistically significant relationship between HA satisfaction and demographic factors, including economic status, type of HA used, and daily HA usage. Elderly individuals with a favorable economic status reported a mean HA satisfaction score, indicating higher satisfaction levels. This finding suggests that individuals with higher economic status, the elderly, or their families tend to experience greater satisfaction with their hearing aids (HAs). Among the elderly participants, 80% used digital hearing aids, and their mean satisfaction with these devices was notably high. This high satisfaction can be attributed to several advantages of digital HAs, including their ability to adapt to various conditions and environments, tailor audio settings to individual needs, reduce wind-induced whistling sounds, maintain a smaller and lighter form factor compared to analog HAs, and automatically adjust ambient sounds to optimize audio quality. The duration of daily HA use showed a significant statistical relationship with HA satisfaction, with individuals using HAs for 8-16 hours reporting high satisfaction. This finding is consistent with the results of previous studies by Romanet et al. (2018), McPherson (2018), and Dashti et al., all of whom reported higher satisfaction scores among individuals using their HAs for more than 4 hours (15, 16, 18).
The present study indicated that hearing assistive devices contribute to an enhanced quality of life among the elderly. The mean quality of life score for elderly individuals in this study was relatively high, consistent with the findings of a study which indicated increased use of hearing assistive devices positively affects physical health and overall quality of life (17).
The results further demonstrated that among the demographic variables, age and quality of life in elderly individuals with hearing loss exhibited a significant statistical association. The mean quality of life score was highest in ages 60-74, with scores declining as individuals grew older. This observation corresponds with the findings of Kateifidis et al. (2017) (17), who reported a Pearson correlation coefficient of -0.43 between age and quality of life. According to research from other countries, hearing loss has been associated with increased dependence and more significant caregiving needs in the elderly, ultimately diminishing their quality of life.
Regarding education levels, the mean HA satisfaction score indicated that as education levels rise among the elderly, HA satisfaction tends to increase. However, there was a slight decrease in satisfaction in the group with higher diploma education, possibly due to other influencing factors and differing expectations regarding satisfaction. Nevertheless, this association did not reach statistical significance. The mean HA satisfaction score among married elderly individuals suggested they were more fulfilled in their daily lives and social activities. Nonetheless, this relationship was not statistically significant.
The number of background diseases in elderly individuals showed a statistically significant relationship with quality of life. As the number of background diseases increased, the mean quality of life score decreased. This research highlighted that a background disease, coupled with hearing loss, can significantly impact the quality of life of elderly individuals. Elderly individuals with hearing loss often require support from their family members. Diseases such as diabetes, cardiovascular disease, and stroke intensify this need, requiring caregivers to be more involved in the elderly individuals' daily activities and increasing their dependence. However, hearing assistive devices can substantially reduce this dependence and improve the quality of life. These findings are consistent with the studies conducted by Romanet et al. and Hussenoeder et al. (18, 19).
Conclusion
In the present study, no tangible relationship was observed between satisfaction with hearing aid use and the mean score of quality of life. However, utilizing hearing-assisting devices, such as hearing aids, has enhanced satisfaction and improved the quality of life among the elderly. As a result, increased engagement in daily activities can enhance their quality of life. Therefore, it is recommended to provide elderly individuals with education on the proper use of hearing aids to improve their quality of life further.
Acknowledgement
This manuscript is based on a master's thesis on elderly nursing approved by the Faculty of Nursing and Midwifery and the Nursing Research Center at Golestan University of Medical Sciences. We sincerely appreciate all the officials and staff of Gorgan Health Insurance and the elderly individuals who assisted us in conducting this study.
Funding sources
This study received financial support from Golestan University of Medical Sciences, Iran.
Ethical statement
The current research received approval from the Ethics Committee of Golestan University of Medical Sciences (Code IR.GUOMS.REC.1398.028). All ethical considerations were diligently observed, such as obtaining a permission letter from the Golestan Health Insurance Office, securing informed written consent and ensuring anonymity.
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Author contributions
All authors contributed to the study design and manuscript preparation; data collection was only performed by the first author and data analysis was performed by the fourth author.
Type of study: Original Article |
Subject:
Nursing
References
1. Kozlowski L, Ribas A, Almeida G, Luz I. Satisfaction of Elderly Hearing Aid Users Int Arch Otorhinolaryngol. 2017;21(1):92-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Cunningham LL, Tucci DL. Hearing Loss in Adults. N Engl J Med. 2017;377(25):2465-73. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Turton L, Souza P, Thibodeau L, Hickson L, Gifford R, Bird J, et al. Guidelines for Best Practice in the Audiological Management of Adults with Severe and Profound Hearing Loss. Semin Hear. 2020;41(3):141-246. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Kim S, Park JM, Han JS, Seo JH, DHan K, Joo YH, et al. Age-related hearing loss in the Korea National Health and Nutrition Examination Survey. PLoS ONE. 2020;15(12):e0243001. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Davis A, McMahon CM, Pichora-Fuller KM, Russ S, Lin F, Olusanya BO, et al. Aging and hearing health: the life-course approach. Gerontologist. 2016;56(Suppl_2):S256-67. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Kim Gy, Cho YS, Byun HM, Seol HY, Lim J, Park JG, et al. Factors Influencing Hearing Aid Satisfaction in South Korea. Yonsei Med J. 2022;63(6):570-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Picou EM. Hearing Aid Benefit and Satisfaction Results from the MarkeTrak 2022 Survey: Importance of Features and Hearing Care Professionals. Semin Hear. 2022;43(4):301-16. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Karaca A, Durna Z. Patient satisfaction with the quality of nursing care. Nurs Open. 2019;6(2):535-45. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. EM Picou. MarkeTrak 10 (MT10) Survey Results Demonstrate High Satisfaction with and Benefits from Hearing Aids. Semin Hear. 2020;41(1):21-36. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Haraldstad K, Wahl A, Andenæs R, Andersen JR, Andersen MH, Beisland E, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. 2019;28(10):2641-50. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Pouyandeh MH, Hoseinabadi R. Factors Influencing the Hearing Aids Use and Satisfaction: A Review Study. Journal of Modern Rehabilitation. 2019;13(3):137-46. [View at Publisher] [DOI] [Google Scholar]
12. McMahon CM, Mosley CL, Pichora-Fuller MK, Davis AC, Baylor CR, Yorkston KM, et al. Older adults' perceptions of current and future hearing healthcare services in Australia, England, US and Canada. Public Health Res Pract. 2021;31(5):3152128. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Khiavi FF, Bayat A, Dashti R, Sameni SJ. Hearing aid-related satisfaction based on type and degree of hearing loss in elderly. Audiology. 2015;23(6):114-22. [View at Publisher] [Google Scholar]
14. Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S. The Iranian Version of 12- item Short Form Health Survey (SF-12): factor structure, internal consistency and construct validity. BMC Public Health. 2009;9(1):341. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Dashti R, Faraji-Khiavi F, Sameni SJ, Bayat A. Satisfaction with Hearing Aids among Aged Patients with Different Degrees of Hearing Loss and Length of Daily Use. J Audiol Otol. 2015;19(1):14-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. McPherson B. Self-Reported Benefit and Satisfaction with a Beamforming Body-Worn Hearing Aid for Elderly Adults. Int J Otolaryngol. 2018;2018:1-14. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Kateifidis N, Sarafis P, Malliarou M, Tsounis A, Bamidis P, Niakas D. Quality of Life and Satisfaction among Patients Who Use Hearing Aids. Glob J Health Sci. 2017;9(6):177. [View at Publisher] [DOI] [Google Scholar]
18. Romanet P, Guy M, Allaert FA. Clinical study on the efficacy, acceptance, and safety of hearing aids in patients with mild to moderate presbyacusis. Panminerva Med. 2018;60(3):92-100. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Hussenoeder FS, Jentzsch D, Matschinger H, Hinz A, Kilian R, Heller SR, et al. Depression and quality of life in old age: a closer look. Eur J Ageing. 2020;18(1):75-83. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






