Abbas Ebadi1 

 , Hadis Ashrafizadeh2
, Hadis Ashrafizadeh2 

 , Leila Khanali Mojen3
, Leila Khanali Mojen3 

 , Somayeh Mirzaie4
, Somayeh Mirzaie4 
 , Zeynab Kazemzadeh4
, Zeynab Kazemzadeh4 
 , Parastoo Ariamloo4
, Parastoo Ariamloo4 

 , Maryam Rassouli5
, Maryam Rassouli5 

 , Jeannine M. Brant6
, Jeannine M. Brant6 




 , Hadis Ashrafizadeh2
, Hadis Ashrafizadeh2 

 , Leila Khanali Mojen3
, Leila Khanali Mojen3 

 , Somayeh Mirzaie4
, Somayeh Mirzaie4 
 , Zeynab Kazemzadeh4
, Zeynab Kazemzadeh4 
 , Parastoo Ariamloo4
, Parastoo Ariamloo4 

 , Maryam Rassouli5
, Maryam Rassouli5 

 , Jeannine M. Brant6
, Jeannine M. Brant6 


1- Behavioral Sciences Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran; Faculty of Nursing, Baqiyatallah University of Medical Sciences, Tehran, Iran
2- Student Research Committee, Faculty of Nursing, Dezful University of Medical Sciences, Dezful, Iran
3- School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
4- Deputy of Nursing, Ministry of Health and Medical Education, Tehran, Iran
5- Cancer Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran; School of Nursing, College of Health Sciences, University of Nizwa, Nizwa, Sultanate of Oman ,Rassouli.m@gmail.com
6- Clinical Science and Innovation, City of Hope, Duarte, California, United States of America
2- Student Research Committee, Faculty of Nursing, Dezful University of Medical Sciences, Dezful, Iran
3- School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
4- Deputy of Nursing, Ministry of Health and Medical Education, Tehran, Iran
5- Cancer Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran; School of Nursing, College of Health Sciences, University of Nizwa, Nizwa, Sultanate of Oman ,
6- Clinical Science and Innovation, City of Hope, Duarte, California, United States of America
Keywords: Quality of health care, Nursing, Action research, Iran, Magnet hospital recognition program
Full-Text [PDF 496 kb]
(100 Downloads)
| Abstract (HTML) (392 Views)
Results
Stage 1: Designing
To initially launch the Outstanding Hospital project, the nursing department sent a letter to 14 universities of medical sciences in Iran. Each of the 14 universities was then asked to introduce one of their hospitals as a pilot hospital and provide a list of processes that nurses were performing but which were irrelevant to nursing care (i.e., practices outside the scope of nursing) (20).
After submitting the reports of irrelevant nursing care practices, all items were categorized along with their frequencies. Finally, three of the most frequent processes were selected: 1) nurses obtaining informed consent, 2) nurses conducting laboratory sampling in non-emergency situations, and 3) nurses coordinating and scheduling follow-up for medical consultations. The request to remove these processes from nursing care was communicated to these centers over a 3-month period. The following programs and solutions facilitated this process.
The current process for informed consent was examined by the hospital’s specialty committee. Informed consent training was provided to medical students and professors by the Education Department and Medical School Faculty, including communication about the legal responsibility of physicians in obtaining informed consent, followed by training nurses about the legal and judicial outcomes of this process.
To remove non-emergency sampling from nursing duties, experienced nurses trained laboratory staff to collect samples, especially in pediatric wards. Nurses received allocation bonuses for sampling and overtime work during the transition period until the required manpower of the laboratory unit was secured. Purchasing equipment such as a labeling machine for the laboratory unit was also arranged to reduce the workload of the laboratory staff and allow them time to collect samples.
Regarding the coordination and scheduling of medical consultations, the following actions were taken: physicians were mandated to accept legal responsibility for providing medical consultations inside the hospital. A contract was also created with specialist physicians outside the hospital to offer requested consultations, a system was designed for registering and notifying physicians, stages of notifying physicians were tracked and recorded, consultations were offered by one of the supervisors in the hospital’s nursing service office, and the results of each step of the process were documented.
Instrument: Upon completion of the first phase-modifying three identified processes-the Deputy of Nursing continued the project in alignment with the Magnet Hospital Model. Six hospitals met the eligibility criteria to advance to implementation. Progression was contingent upon verified compliance with benchmarks, specifically eliminating three operational procedures inconsistent with nursing job descriptions.
One of the prerequisites for inclusion in this next project was the completion of the International Intervention Hospital Magnet Gap Analysis Tool (21), which was sent to the Nursing Department along with a questionnaire titled Hospital Identification Card and the approval of the university’s nursing managers for implementation of the project. The project was funded by the Deputy of Nursing of the MOH.
The International Intervention Hospital Magnet Gap Analysis Tool and a Hospital Identification Card were used. The tool consisted of 77 items on a 4-point Likert scale (0 = no development, 1 = in development, 2 = dissemination, 3 = enculturation) in seven dimensions: eligibility requirements (9 items), organizational overview (11 items), empirical outcomes (1 general item), transformational leadership (10 items), structural empowerment (15 items), exemplary professional practice (24 items), and new knowledge/innovations (7 items). The tool was translated and culturally adjusted, reducing items to 53 due to contextual differences between Iran and the USA.
The Hospital Identification Card evaluated human resources within each center, including staff numbers, distribution, educational qualifications, and work experience. This analysis was crucial for estimating workforce needs and addressing shortages.
The International Intervention Hospital Magnet Gap Analysis Tool was first translated and culturally adjusted by a team of policymakers and experts in the field of healthcare and nursing. Accordingly, the number of items was reduced to 53 due to differences in the nursing context between Iran and the USA.
After collecting data related to the International Intervention Hospital Magnet Gap Analysis Tool, a one-year operational plan was developed by a team of Ministry experts, two faculty members with executive experience, the university’s nursing director, and the hospital’s nursing director. A Gantt chart for implementation of the plan was communicated, and evaluation indicators of the program were determined. In the dimension of organizational overview, the percentage of updates to the hospital website and management information dashboard were considered. Under empirical outcomes, indicators such as the percentage and frequency of falls, ulcers, patient education, use of nursing diagnoses, pain management, and patient satisfaction were taken into account. For transformational leadership, the analysis of received reports was examined. Within the structural empowerment dimension, the percentage of nurses who obtained their professional competence license was noted. Finally, in the dimension of new knowledge and innovations, research in human resources, electronic nursing documentation, and the reporting system were evaluated as outcomes.
Stage 2: Implementation
Measures taken to develop and promote infrastructure in pilot hospitals reflective of the Magnet Model, which were planned in the previous stage, were implemented as follows:
Full-Text: (33 Views)
Introduction
Quality nursing care is defined as addressing human needs through attention, empathy, respectful interactions with the patient, a sense of responsibility, and integrated support for the care seeker (1). In addition, care should be purposeful, using the nursing process, patient satisfaction, and care provision with science and knowledge (2). The health system has an additional responsibility to deliver high-quality care. Leaders of healthcare organizations are challenged to re-examine the quality of nursing care on an ongoing basis (3). The demand for improved healthcare quality is on the rise due to reports of substandard care, increased clients’ attention to and demand for quality care, professional concerns about patient care outcomes, and the sensitivity and efforts of insurers and other payers to control service delivery costs (4). This is despite the fact that in recent years, the shortage of nurses and their increased workload have had a significant impact on the quality of nursing care (5) and have created concerns about patient safety (3). Therefore, in many cases, the quality of nursing care is a cornerstone for grading and accreditation of hospitals (6).
Since the quality of nursing services is a major contributor to the sustainability and success of the health system, various approaches have been introduced to improve the quality of nursing services, such as the Donabedian model and the Magnet Hospital Recognition Program (7). Donabedian presented a model with three parts: structure, process, and output to measure the quality of health services. Accordingly, in any quality improvement program, these three elements should be combined to achieve a suitable result (8). Another model to improve the quality of nursing care is the Magnet Hospital Recognition Program, which refers to a hospital designated by the American Nurses Credentialing Center as a provider of the highest level of nursing care quality (9). This center has classified five essential components within a Magnet hospital to achieve success. These components include 1) transformational leadership, 2) structural empowerment, 3) exemplary professional practice, 4) new knowledge, innovation, and improvements, and 5) empirical quality outcomes (10).
The organizational structures of Magnet hospitals are associated with better prognoses for patients, increased patient satisfaction, better clinical experiences and outcomes, increased autonomy and authority, and subsequently improved job satisfaction among nurses, which leads to their empowerment (11-13). Therefore, considering the complexity of the nurse shortage and the need to consider factors affecting recruitment, retention, and efficiency, this model is also important in addressing the challenge of the nurse shortage (14), which aligns with the current situation in Iran.
In recent years, new care needs required the implementation of some basic and fundamental changes in nursing. A framework was developed to guarantee the provision of safe nursing care, improve optimal performance, prevent poor performance, and predict necessary measures to modify processes and empower patients to evaluate the adequacy of nursing care, because nurse–patient interactions during the provision of direct care are usually considered an indicator of effective care.
In response to this framework, the Deputy of Nursing in Iran has carried out several activities to continue improvements in service provision (15). One of these programs is the Outstanding Hospital project, which was launched to address people’s needs for receiving quality nursing services in Iran. The project aims to improve NSIs such as pressure ulcers, falls, pain management, and satisfaction in selected hospitals. Improving nurses’ ability to accelerate patients’ recovery and their return to home and family is an important factor (16). On the other hand, increasing the hours of direct nursing care has had an impact on patient satisfaction, which directed the focus of this project towards nurses’ job descriptions and the elimination of irrelevant processes (17).
Since using the Magnet title required obtaining relevant permits from the competent authorities and implementing the program in full detail with the approval of the organization that owned the project’s ownership rights, and due to obstacles such as sanctions, it was not possible to obtain permits. Therefore, this project was implemented under the title “Outstanding Hospital Project” and in the form of a relative model of Magnet.
The Outstanding Hospital project in Iran was launched in July 2022 with the aim of standardizing nursing-related processes to improve the quality of nursing care within clinical settings. This paper provides a brief report of a feasibility study conducted as a pilot action research project by the Deputy of Nursing of the Ministry of Health & Medical Education.
Methods
In order to assess the feasibility of implementing the Magnet Hospital Recognition Project in the country, participatory action research was conducted based on the approach proposed by McNiff. Action research, by combining research with action, can help improve services and empower service providers in healthcare and hospital settings (18). The main stages of all action research studies are design, implementation, evaluation, and finally institutionalization of the action (19).
Study design
This study employed an action research approach conducted across selected universities of medical sciences in Iran between July 2022 and July 2024.
Study sample and setting
The study population comprised all hospitals affiliated with universities of medical sciences nationwide. From this group, six universities were selected as the study sample for implementing the Magnet Hospital plan, based on inclusion criteria determined by the Deputy of Nursing.
The selection criteria for these hospitals included having a nearly-standard number of nursing staff, an excellent score in accreditation, coordination between hospital managers and nursing management, and adequate facilities and equipment. Accordingly, six hospitals were selected: Imam Khomeini Hospital (Tehran), Namazi Hospital (Shiraz), Shahid Rahimi Hospital (Khorram Abad), Shahid Bahonar Hospital (Kerman), Mardani Azar Hospital (Tabriz), and Imam Reza Hospital (Kermanshah).
Study procedure:
In this study, a three-stage cycle of action research was implemented over 2 years. Each stage consisted of two steps, meaning the three general stages were divided into six steps. Figure 1 shows the action research process and the steps taken.
Stage one (Designing): This stage consisted of two steps: identifying needs and planning for change. After identifying the problem at the hospital level through document reviews, field visits, and reports of patient and nurse dissatisfaction, the Deputy of Nursing prepared an implementation plan. After obtaining official permission from the selected hospitals to conduct the pilot project, additional information, data collection, and planning were carried out.
Stage two (Implementation): This stage included two steps: implementation and reflection. Based on findings from the first stage, the research team resolved obstacles and provided the necessary facilities and equipment for corrective actions, preparing conditions for the pilot program's implementation. With the start of the program and its initial implementation, project progress reports were provided every 3 months through verbal updates, online meetings, and written documentation. After 6 months, a field visit was conducted to identify areas for improvement and potential challenges, leading to decisions about program modifications.
Stage three (Evaluation): This stage included evaluation and institutionalization steps. Due to the temporary suspension of the project caused by implementation challenges, the final institutionalization stage has not yet been completed.
In this action research, implementation and evaluation were carried out simultaneously, intertwining the stages. Therefore, the project method and findings are presented narratively and side by side.
Quality nursing care is defined as addressing human needs through attention, empathy, respectful interactions with the patient, a sense of responsibility, and integrated support for the care seeker (1). In addition, care should be purposeful, using the nursing process, patient satisfaction, and care provision with science and knowledge (2). The health system has an additional responsibility to deliver high-quality care. Leaders of healthcare organizations are challenged to re-examine the quality of nursing care on an ongoing basis (3). The demand for improved healthcare quality is on the rise due to reports of substandard care, increased clients’ attention to and demand for quality care, professional concerns about patient care outcomes, and the sensitivity and efforts of insurers and other payers to control service delivery costs (4). This is despite the fact that in recent years, the shortage of nurses and their increased workload have had a significant impact on the quality of nursing care (5) and have created concerns about patient safety (3). Therefore, in many cases, the quality of nursing care is a cornerstone for grading and accreditation of hospitals (6).
Since the quality of nursing services is a major contributor to the sustainability and success of the health system, various approaches have been introduced to improve the quality of nursing services, such as the Donabedian model and the Magnet Hospital Recognition Program (7). Donabedian presented a model with three parts: structure, process, and output to measure the quality of health services. Accordingly, in any quality improvement program, these three elements should be combined to achieve a suitable result (8). Another model to improve the quality of nursing care is the Magnet Hospital Recognition Program, which refers to a hospital designated by the American Nurses Credentialing Center as a provider of the highest level of nursing care quality (9). This center has classified five essential components within a Magnet hospital to achieve success. These components include 1) transformational leadership, 2) structural empowerment, 3) exemplary professional practice, 4) new knowledge, innovation, and improvements, and 5) empirical quality outcomes (10).
The organizational structures of Magnet hospitals are associated with better prognoses for patients, increased patient satisfaction, better clinical experiences and outcomes, increased autonomy and authority, and subsequently improved job satisfaction among nurses, which leads to their empowerment (11-13). Therefore, considering the complexity of the nurse shortage and the need to consider factors affecting recruitment, retention, and efficiency, this model is also important in addressing the challenge of the nurse shortage (14), which aligns with the current situation in Iran.
In recent years, new care needs required the implementation of some basic and fundamental changes in nursing. A framework was developed to guarantee the provision of safe nursing care, improve optimal performance, prevent poor performance, and predict necessary measures to modify processes and empower patients to evaluate the adequacy of nursing care, because nurse–patient interactions during the provision of direct care are usually considered an indicator of effective care.
In response to this framework, the Deputy of Nursing in Iran has carried out several activities to continue improvements in service provision (15). One of these programs is the Outstanding Hospital project, which was launched to address people’s needs for receiving quality nursing services in Iran. The project aims to improve NSIs such as pressure ulcers, falls, pain management, and satisfaction in selected hospitals. Improving nurses’ ability to accelerate patients’ recovery and their return to home and family is an important factor (16). On the other hand, increasing the hours of direct nursing care has had an impact on patient satisfaction, which directed the focus of this project towards nurses’ job descriptions and the elimination of irrelevant processes (17).
Since using the Magnet title required obtaining relevant permits from the competent authorities and implementing the program in full detail with the approval of the organization that owned the project’s ownership rights, and due to obstacles such as sanctions, it was not possible to obtain permits. Therefore, this project was implemented under the title “Outstanding Hospital Project” and in the form of a relative model of Magnet.
The Outstanding Hospital project in Iran was launched in July 2022 with the aim of standardizing nursing-related processes to improve the quality of nursing care within clinical settings. This paper provides a brief report of a feasibility study conducted as a pilot action research project by the Deputy of Nursing of the Ministry of Health & Medical Education.
Methods
In order to assess the feasibility of implementing the Magnet Hospital Recognition Project in the country, participatory action research was conducted based on the approach proposed by McNiff. Action research, by combining research with action, can help improve services and empower service providers in healthcare and hospital settings (18). The main stages of all action research studies are design, implementation, evaluation, and finally institutionalization of the action (19).
Study design
This study employed an action research approach conducted across selected universities of medical sciences in Iran between July 2022 and July 2024.
Study sample and setting
The study population comprised all hospitals affiliated with universities of medical sciences nationwide. From this group, six universities were selected as the study sample for implementing the Magnet Hospital plan, based on inclusion criteria determined by the Deputy of Nursing.
The selection criteria for these hospitals included having a nearly-standard number of nursing staff, an excellent score in accreditation, coordination between hospital managers and nursing management, and adequate facilities and equipment. Accordingly, six hospitals were selected: Imam Khomeini Hospital (Tehran), Namazi Hospital (Shiraz), Shahid Rahimi Hospital (Khorram Abad), Shahid Bahonar Hospital (Kerman), Mardani Azar Hospital (Tabriz), and Imam Reza Hospital (Kermanshah).
Study procedure:
In this study, a three-stage cycle of action research was implemented over 2 years. Each stage consisted of two steps, meaning the three general stages were divided into six steps. Figure 1 shows the action research process and the steps taken.
Stage one (Designing): This stage consisted of two steps: identifying needs and planning for change. After identifying the problem at the hospital level through document reviews, field visits, and reports of patient and nurse dissatisfaction, the Deputy of Nursing prepared an implementation plan. After obtaining official permission from the selected hospitals to conduct the pilot project, additional information, data collection, and planning were carried out.
Stage two (Implementation): This stage included two steps: implementation and reflection. Based on findings from the first stage, the research team resolved obstacles and provided the necessary facilities and equipment for corrective actions, preparing conditions for the pilot program's implementation. With the start of the program and its initial implementation, project progress reports were provided every 3 months through verbal updates, online meetings, and written documentation. After 6 months, a field visit was conducted to identify areas for improvement and potential challenges, leading to decisions about program modifications.
Stage three (Evaluation): This stage included evaluation and institutionalization steps. Due to the temporary suspension of the project caused by implementation challenges, the final institutionalization stage has not yet been completed.
In this action research, implementation and evaluation were carried out simultaneously, intertwining the stages. Therefore, the project method and findings are presented narratively and side by side.
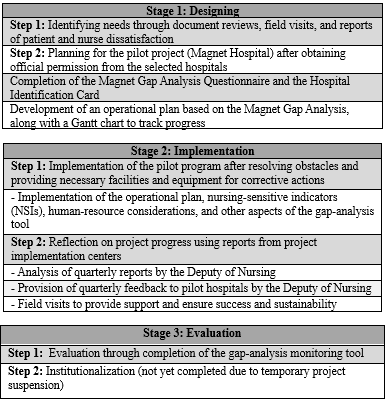 Figure 1. The action research process |
Results
Stage 1: Designing
To initially launch the Outstanding Hospital project, the nursing department sent a letter to 14 universities of medical sciences in Iran. Each of the 14 universities was then asked to introduce one of their hospitals as a pilot hospital and provide a list of processes that nurses were performing but which were irrelevant to nursing care (i.e., practices outside the scope of nursing) (20).
After submitting the reports of irrelevant nursing care practices, all items were categorized along with their frequencies. Finally, three of the most frequent processes were selected: 1) nurses obtaining informed consent, 2) nurses conducting laboratory sampling in non-emergency situations, and 3) nurses coordinating and scheduling follow-up for medical consultations. The request to remove these processes from nursing care was communicated to these centers over a 3-month period. The following programs and solutions facilitated this process.
The current process for informed consent was examined by the hospital’s specialty committee. Informed consent training was provided to medical students and professors by the Education Department and Medical School Faculty, including communication about the legal responsibility of physicians in obtaining informed consent, followed by training nurses about the legal and judicial outcomes of this process.
To remove non-emergency sampling from nursing duties, experienced nurses trained laboratory staff to collect samples, especially in pediatric wards. Nurses received allocation bonuses for sampling and overtime work during the transition period until the required manpower of the laboratory unit was secured. Purchasing equipment such as a labeling machine for the laboratory unit was also arranged to reduce the workload of the laboratory staff and allow them time to collect samples.
Regarding the coordination and scheduling of medical consultations, the following actions were taken: physicians were mandated to accept legal responsibility for providing medical consultations inside the hospital. A contract was also created with specialist physicians outside the hospital to offer requested consultations, a system was designed for registering and notifying physicians, stages of notifying physicians were tracked and recorded, consultations were offered by one of the supervisors in the hospital’s nursing service office, and the results of each step of the process were documented.
Instrument: Upon completion of the first phase-modifying three identified processes-the Deputy of Nursing continued the project in alignment with the Magnet Hospital Model. Six hospitals met the eligibility criteria to advance to implementation. Progression was contingent upon verified compliance with benchmarks, specifically eliminating three operational procedures inconsistent with nursing job descriptions.
One of the prerequisites for inclusion in this next project was the completion of the International Intervention Hospital Magnet Gap Analysis Tool (21), which was sent to the Nursing Department along with a questionnaire titled Hospital Identification Card and the approval of the university’s nursing managers for implementation of the project. The project was funded by the Deputy of Nursing of the MOH.
The International Intervention Hospital Magnet Gap Analysis Tool and a Hospital Identification Card were used. The tool consisted of 77 items on a 4-point Likert scale (0 = no development, 1 = in development, 2 = dissemination, 3 = enculturation) in seven dimensions: eligibility requirements (9 items), organizational overview (11 items), empirical outcomes (1 general item), transformational leadership (10 items), structural empowerment (15 items), exemplary professional practice (24 items), and new knowledge/innovations (7 items). The tool was translated and culturally adjusted, reducing items to 53 due to contextual differences between Iran and the USA.
The Hospital Identification Card evaluated human resources within each center, including staff numbers, distribution, educational qualifications, and work experience. This analysis was crucial for estimating workforce needs and addressing shortages.
The International Intervention Hospital Magnet Gap Analysis Tool was first translated and culturally adjusted by a team of policymakers and experts in the field of healthcare and nursing. Accordingly, the number of items was reduced to 53 due to differences in the nursing context between Iran and the USA.
After collecting data related to the International Intervention Hospital Magnet Gap Analysis Tool, a one-year operational plan was developed by a team of Ministry experts, two faculty members with executive experience, the university’s nursing director, and the hospital’s nursing director. A Gantt chart for implementation of the plan was communicated, and evaluation indicators of the program were determined. In the dimension of organizational overview, the percentage of updates to the hospital website and management information dashboard were considered. Under empirical outcomes, indicators such as the percentage and frequency of falls, ulcers, patient education, use of nursing diagnoses, pain management, and patient satisfaction were taken into account. For transformational leadership, the analysis of received reports was examined. Within the structural empowerment dimension, the percentage of nurses who obtained their professional competence license was noted. Finally, in the dimension of new knowledge and innovations, research in human resources, electronic nursing documentation, and the reporting system were evaluated as outcomes.
Stage 2: Implementation
Measures taken to develop and promote infrastructure in pilot hospitals reflective of the Magnet Model, which were planned in the previous stage, were implemented as follows:
- Empowering managers at different levels regarding general and specialty nursing management skills through a 3-day training workshop
- Updating the hospital websites and strategic plans of the hospitals in line with the organizational overview.
- Developing and implementing training courses for using the nursing process focused on nursing diagnoses, as well as developing pain management and wound management courses for all centers. These trainings were planned as part of a mentorship program. First, middle managers, including supervisors and head nurses, and some experienced or competent nurses in each hospital were trained by faculty members; training then continued in the centers by these individuals under the supervision of faculty members so that all nurses could receive the necessary training.
- Completion of a patient satisfaction online survey, along with in-person patient education and follow-up, in line with the empirical outcomes dimension
- Designing and communicating a data dashboard to record points/scores of NSIs, developing and implementing an operational plan, and creating a quarterly review of related trends by nursing managers in line with transformational leadership.
- Facilitating the process for nurses to receive a professional competence license in line with structural empowerment.
- Forming an evidence-based practice and research committee with the Dean of the nursing school of that province, faculty members, managers, and qualified nurses of the pilot center in line with new knowledge and innovations. The first research project of this committee was aimed at examining the nursing workforce according to the World Health Organization WISN method. At this stage of the proposal, hours of direct care have been determined, and indirect care and personal activities have been approved and are being implemented.
- Implementing the plan for initiating electronic nursing documentation and reporting based on nursing diagnoses, to reduce indirect care hours and increase report accuracy, in line with the dimension of new knowledge and innovations.
For reflection, both in-person and online meetings were held with project participants, including matrons, supervisors, head nurses, nurses of the centers, and the hospital director. These meetings were conducted in the form of field visits and online sessions. The purpose of these meetings was to provide feedback on the implementation process and progress made, and to identify challenges and potential issues.
Stage 3: Evaluation
The completion of the gap analysis monitoring tool (In five dimensions) showed the progress of the program and the effectiveness of its implementation in some dimensions. Since the project was not completed, the final analysis of the data and the results of the statistical analyses could not be presented; therefore, the results were presented in a qualitative manner.
In the organizational overview dimension, all strategic plans were placed on the websites of the three hospitals. In the empirical outcome dimension, improved clinical outcomes included enhanced patient satisfaction and patient education. Pain management was implemented in one center. The wound management course has not yet been implemented in any center. However, no significant changes were reported in the fall and pressure ulcer indicators. In the transformational leadership dimension, the previously developed information dashboard was analyzed and operational plans performed. In the structural empowerment dimension, obtaining professional competence licenses increased by about 20% across all centers. In the new knowledge and innovations dimension, the proposal obtained the code of ethics, and sampling and analysis of the findings were performed. The results will be presented in future seminars, as well as in the periodic meetings of nursing managers in the country and published in journals. Additionally, regarding the establishment of the electronic nursing documentation and reporting system in one hospital, 50% progress has been achieved.
Discussion
Considering the necessity of improving the quality of nursing care as the ultimate goal of the Deputy of Nursing, and the importance of Magnet hospitals in enhancing these services, a feasibility study was conducted to implement the Magnet Hospitals project in Iran in three stages.
In the first stage, following the needs assessment, the cooperation of all managers at various levels of the university and hospital, as well as hospital nurses, was sought to implement the Magnet model in the pilot hospitals. Svensson et al. described the implementation of the Magnet model under the theme "Creating space for magnet" in a qualitative study. In this category, involving all personnel in the implementation of this model was seen as both crucial and challenging. They believed that engagement at all levels of the hospital (horizontal and vertical) would change the organizational culture and increase the motivation to adopt the new organizational model, which covers all three factors-individual, organizational, and supra-organizational-that should be considered in implementing the Magnet model (22).
Paquay et al. (2021) identified the personal emotions, culture, and beliefs of individuals (23), while Urden et al. (2021) emphasized the commitment of chief nursing officers and senior nurses as crucial factors for the successful implementation of this model (24). Additionally, organizational support, including backing from the head of the center and the board of directors, is important. In this project, support from the highest level of management in various financial, facility, and operational dimensions ensured that these aspects were not significant obstacles for the project. Support from outside the organization was another key achievement, facilitated by cooperation with the nursing schools. Given that one of the primary concerns of nursing schools and managers is providing efficient human resources, the project implementation was also important for them.
The second stage of implementing the Magnet model was carried out in accordance with the designed indicators for each dimension. One of the challenges experienced in this phase was the shortage of nursing staff. Previous studies also highlighted the shortage of staff as a significant issue for the implementation and development of this model (22,23). In a qualitative study, participants noted that although the idea of the Magnet model is very attractive and beneficial, the staffing situation is problematic. Paquay et al. also identified the shortage of nursing staff as an obstacle to implementing the Magnet model in Belgium and emphasized the importance of managing nursing staff in a humane and non-bureaucratic manner (23).
One of the five key dimensions was empirical outcomes, which were measured using nursing-sensitive indicators (NSIs). In this project, five indicators were considered to evaluate the quality of nursing care. In the Magnet hospital in Germany, falls with injury and pressure ulcers were among the NSIs. The development of these indicators in North America, including the U.S. and Canada, was noted, while the limitations of these indicators in Germany were identified as a significant challenge in their Magnet hospitals, underscoring the need for their development in Germany (25). In Australia, the indicators include clinical training readiness, burnout, job satisfaction, and intention to leave the job. Therefore, these indicators vary across different countries and settings (13). NSIs are crucial in enhancing the quality of care and improving patient outcomes (26). Although the current study did not demonstrate statistically significant improvements across all measured indicators, this outcome is not unexpected given the program's early implementation phase and the inherent complexity of systemic change in healthcare settings. As a nationwide feasibility study, the scope was designed to assess operational viability rather than deliver immediate outcome-based transformations. In this context, the observed increase in patient satisfaction is a meaningful success, particularly as it reflects the responsiveness of patients to initial interventions.
It is important to acknowledge that transformational initiatives, such as those grounded in the Magnet Hospital Model, require sustained effort and longitudinal evaluation to capture their full impact. The results presented here represent only a single pilot cycle within a broader long-term project. Therefore, drawing conclusions about the program's effectiveness must be approached cautiously, with recognition of the phased nature of implementation.
Moreover, challenges in indicator reporting-especially in relation to patient safety metrics such as fall incidents-may have further influenced the findings. Previous research and operational audits have identified underreporting as a systemic issue in several countries, including Iran. Cultural, institutional, and procedural factors often contribute to reporting gaps, which may obscure the true prevalence of adverse events and hinder accurate assessment of quality improvement efforts. Although this study did not show significant changes in some indicators, the increase in patient satisfaction represents a significant success. Numerous sources emphasize the importance of patient satisfaction as the primary indicator of service evaluation in nursing (27,28). The involvement of nursing managers in designing, participating in data analysis, and revising the operational plan to achieve project goals is a key factor in this success. Asgari et al., in assessing the readiness of a teaching hospital in Yazd for the Magnet model in Iran, highlighted the importance of managerial attention to the professional development of nurses, resulting in positive professional progress (29). However, Maier also noted delays in achieving goals due to inadequate infrastructure, such as the need for electronic nursing documentation. The impact of electronic reporting on nursing workload presents a similar challenge in some countries (25). Another achievement of this program is conducting research by the nursing management department in collaboration with nursing school faculty members, which not only enhances the research skills of clinical nurses but also fosters greater cooperation and support from schools for clinical practices-an important Magnet project indicator. A work sampling study designed in the present project aims to estimate the required manpower in the centers based on the Wilson formula (Direct and indirect care), with participation from nursing management and university nursing schools involved in the project.
As the project is still ongoing, benchmarking remains a crucial step in demonstrating the effectiveness of the Magnet project. Since most of the scores obtained from the gap analysis questionnaire were 1, with very few being 2, it appears that the pilot hospitals of the project are still in the planning stages to achieve the standards. According to the classification provided, a score of 1 (In development) means that the standard requirements are in the planning and development stage, with no implementation carried out. A score of 2 (Disseminated) indicates that the standard requirements are fully developed and are being implemented and disseminated within the organization.
Conclusion
The Magnet Recognition Program is regarded as the superior standard for evidence-based nursing practice and encourages nurses to exercise effective leadership while improving the quality of medical treatment and patient care. To promote quality nursing care, quality improvement models such as the Magnet Recognition Program should be considered to remove obstacles and establish a framework for planning. The model hospital project is being implemented as a pilot project aimed at improving the quality of nursing care in line with the philosophy and principles of the Magnet project, focusing on process improvement and nurse empowerment while addressing challenges related to the shortage of nurses. It also seeks to promote NSIs such as patient satisfaction, pain management, fall assessment, patient education, post-discharge follow-up, and pressure ulcer prevention. The organizational structures of Magnet hospitals provide a set of work environment standards that support the professional practice of nursing and empower nurses by increasing autonomy, discretion, and ultimately job satisfaction. To achieve the goals of the model, in addition to emphasizing multidisciplinary and interdisciplinary care, it is necessary to create opportunities for personal growth and development of nurses-particularly novice and beginner nurses-strengthen the focus on evidence-based nursing, incorporate new technologies in care such as telehealth nursing, and plan precise periodic evaluations to monitor the program’s effectiveness.
It should be noted that the Magnet Hospital project is not applicable to all hospitals, as only 10% of U.S. hospitals have received such recognition. Strong infrastructure-such as dedicated nursing management portals, reliable information technology systems, and access to specialized training resources-is essential for implementing this system, but is not available in all hospitals. Therefore, before generalizing our findings, detailed assessments of the infrastructure of candidate hospitals are necessary.
Acknowledgement
Hereby, the authors express their gratitude to all authorities of the six pilot universities of medical sciences in Tehran, Shiraz, Kerman, Kermanshah, Lorestan, and Tabriz, as well as the managers, nurses, and personnel in the pilot hospitals for their outstanding work and cooperation.
Funding sources
No external funding was received. The project was entirely designed, conducted, monitored, and financially supported by the Deputy of Nursing, Ministry of Health and Medical Education.
Ethical statement
Not applicable.
Conflicts of interest
Authors declare no conflicts of interest.
Author contributions
AE: Conceptualization, Methodology, Writing - Original Draft; HA: Data Curation, Validation, Data Analysis, Writing - Original Draft; LKM: Conceptualization, Validation, Data Analysis, Writing - Original Draft; SM, ZK, PA: Investigation, Data Curation, Formal Analysis; MR: Conceptualization, Funding Acquisition, Methodology, Writing - Original Draft, Supervision; JB: Conceptualization, Methodology, Writing - Original Draft, Supervision; All authors reviewed and approved the final manuscript.
Data availability statement
The datasets generated during this study are not publicly available due to confidentiality constraints but can be obtained from the corresponding author upon reasonable request.
Stage 3: Evaluation
The completion of the gap analysis monitoring tool (In five dimensions) showed the progress of the program and the effectiveness of its implementation in some dimensions. Since the project was not completed, the final analysis of the data and the results of the statistical analyses could not be presented; therefore, the results were presented in a qualitative manner.
In the organizational overview dimension, all strategic plans were placed on the websites of the three hospitals. In the empirical outcome dimension, improved clinical outcomes included enhanced patient satisfaction and patient education. Pain management was implemented in one center. The wound management course has not yet been implemented in any center. However, no significant changes were reported in the fall and pressure ulcer indicators. In the transformational leadership dimension, the previously developed information dashboard was analyzed and operational plans performed. In the structural empowerment dimension, obtaining professional competence licenses increased by about 20% across all centers. In the new knowledge and innovations dimension, the proposal obtained the code of ethics, and sampling and analysis of the findings were performed. The results will be presented in future seminars, as well as in the periodic meetings of nursing managers in the country and published in journals. Additionally, regarding the establishment of the electronic nursing documentation and reporting system in one hospital, 50% progress has been achieved.
Discussion
Considering the necessity of improving the quality of nursing care as the ultimate goal of the Deputy of Nursing, and the importance of Magnet hospitals in enhancing these services, a feasibility study was conducted to implement the Magnet Hospitals project in Iran in three stages.
In the first stage, following the needs assessment, the cooperation of all managers at various levels of the university and hospital, as well as hospital nurses, was sought to implement the Magnet model in the pilot hospitals. Svensson et al. described the implementation of the Magnet model under the theme "Creating space for magnet" in a qualitative study. In this category, involving all personnel in the implementation of this model was seen as both crucial and challenging. They believed that engagement at all levels of the hospital (horizontal and vertical) would change the organizational culture and increase the motivation to adopt the new organizational model, which covers all three factors-individual, organizational, and supra-organizational-that should be considered in implementing the Magnet model (22).
Paquay et al. (2021) identified the personal emotions, culture, and beliefs of individuals (23), while Urden et al. (2021) emphasized the commitment of chief nursing officers and senior nurses as crucial factors for the successful implementation of this model (24). Additionally, organizational support, including backing from the head of the center and the board of directors, is important. In this project, support from the highest level of management in various financial, facility, and operational dimensions ensured that these aspects were not significant obstacles for the project. Support from outside the organization was another key achievement, facilitated by cooperation with the nursing schools. Given that one of the primary concerns of nursing schools and managers is providing efficient human resources, the project implementation was also important for them.
The second stage of implementing the Magnet model was carried out in accordance with the designed indicators for each dimension. One of the challenges experienced in this phase was the shortage of nursing staff. Previous studies also highlighted the shortage of staff as a significant issue for the implementation and development of this model (22,23). In a qualitative study, participants noted that although the idea of the Magnet model is very attractive and beneficial, the staffing situation is problematic. Paquay et al. also identified the shortage of nursing staff as an obstacle to implementing the Magnet model in Belgium and emphasized the importance of managing nursing staff in a humane and non-bureaucratic manner (23).
One of the five key dimensions was empirical outcomes, which were measured using nursing-sensitive indicators (NSIs). In this project, five indicators were considered to evaluate the quality of nursing care. In the Magnet hospital in Germany, falls with injury and pressure ulcers were among the NSIs. The development of these indicators in North America, including the U.S. and Canada, was noted, while the limitations of these indicators in Germany were identified as a significant challenge in their Magnet hospitals, underscoring the need for their development in Germany (25). In Australia, the indicators include clinical training readiness, burnout, job satisfaction, and intention to leave the job. Therefore, these indicators vary across different countries and settings (13). NSIs are crucial in enhancing the quality of care and improving patient outcomes (26). Although the current study did not demonstrate statistically significant improvements across all measured indicators, this outcome is not unexpected given the program's early implementation phase and the inherent complexity of systemic change in healthcare settings. As a nationwide feasibility study, the scope was designed to assess operational viability rather than deliver immediate outcome-based transformations. In this context, the observed increase in patient satisfaction is a meaningful success, particularly as it reflects the responsiveness of patients to initial interventions.
It is important to acknowledge that transformational initiatives, such as those grounded in the Magnet Hospital Model, require sustained effort and longitudinal evaluation to capture their full impact. The results presented here represent only a single pilot cycle within a broader long-term project. Therefore, drawing conclusions about the program's effectiveness must be approached cautiously, with recognition of the phased nature of implementation.
Moreover, challenges in indicator reporting-especially in relation to patient safety metrics such as fall incidents-may have further influenced the findings. Previous research and operational audits have identified underreporting as a systemic issue in several countries, including Iran. Cultural, institutional, and procedural factors often contribute to reporting gaps, which may obscure the true prevalence of adverse events and hinder accurate assessment of quality improvement efforts. Although this study did not show significant changes in some indicators, the increase in patient satisfaction represents a significant success. Numerous sources emphasize the importance of patient satisfaction as the primary indicator of service evaluation in nursing (27,28). The involvement of nursing managers in designing, participating in data analysis, and revising the operational plan to achieve project goals is a key factor in this success. Asgari et al., in assessing the readiness of a teaching hospital in Yazd for the Magnet model in Iran, highlighted the importance of managerial attention to the professional development of nurses, resulting in positive professional progress (29). However, Maier also noted delays in achieving goals due to inadequate infrastructure, such as the need for electronic nursing documentation. The impact of electronic reporting on nursing workload presents a similar challenge in some countries (25). Another achievement of this program is conducting research by the nursing management department in collaboration with nursing school faculty members, which not only enhances the research skills of clinical nurses but also fosters greater cooperation and support from schools for clinical practices-an important Magnet project indicator. A work sampling study designed in the present project aims to estimate the required manpower in the centers based on the Wilson formula (Direct and indirect care), with participation from nursing management and university nursing schools involved in the project.
As the project is still ongoing, benchmarking remains a crucial step in demonstrating the effectiveness of the Magnet project. Since most of the scores obtained from the gap analysis questionnaire were 1, with very few being 2, it appears that the pilot hospitals of the project are still in the planning stages to achieve the standards. According to the classification provided, a score of 1 (In development) means that the standard requirements are in the planning and development stage, with no implementation carried out. A score of 2 (Disseminated) indicates that the standard requirements are fully developed and are being implemented and disseminated within the organization.
Conclusion
The Magnet Recognition Program is regarded as the superior standard for evidence-based nursing practice and encourages nurses to exercise effective leadership while improving the quality of medical treatment and patient care. To promote quality nursing care, quality improvement models such as the Magnet Recognition Program should be considered to remove obstacles and establish a framework for planning. The model hospital project is being implemented as a pilot project aimed at improving the quality of nursing care in line with the philosophy and principles of the Magnet project, focusing on process improvement and nurse empowerment while addressing challenges related to the shortage of nurses. It also seeks to promote NSIs such as patient satisfaction, pain management, fall assessment, patient education, post-discharge follow-up, and pressure ulcer prevention. The organizational structures of Magnet hospitals provide a set of work environment standards that support the professional practice of nursing and empower nurses by increasing autonomy, discretion, and ultimately job satisfaction. To achieve the goals of the model, in addition to emphasizing multidisciplinary and interdisciplinary care, it is necessary to create opportunities for personal growth and development of nurses-particularly novice and beginner nurses-strengthen the focus on evidence-based nursing, incorporate new technologies in care such as telehealth nursing, and plan precise periodic evaluations to monitor the program’s effectiveness.
It should be noted that the Magnet Hospital project is not applicable to all hospitals, as only 10% of U.S. hospitals have received such recognition. Strong infrastructure-such as dedicated nursing management portals, reliable information technology systems, and access to specialized training resources-is essential for implementing this system, but is not available in all hospitals. Therefore, before generalizing our findings, detailed assessments of the infrastructure of candidate hospitals are necessary.
Acknowledgement
Hereby, the authors express their gratitude to all authorities of the six pilot universities of medical sciences in Tehran, Shiraz, Kerman, Kermanshah, Lorestan, and Tabriz, as well as the managers, nurses, and personnel in the pilot hospitals for their outstanding work and cooperation.
Funding sources
No external funding was received. The project was entirely designed, conducted, monitored, and financially supported by the Deputy of Nursing, Ministry of Health and Medical Education.
Ethical statement
Not applicable.
Conflicts of interest
Authors declare no conflicts of interest.
Author contributions
AE: Conceptualization, Methodology, Writing - Original Draft; HA: Data Curation, Validation, Data Analysis, Writing - Original Draft; LKM: Conceptualization, Validation, Data Analysis, Writing - Original Draft; SM, ZK, PA: Investigation, Data Curation, Formal Analysis; MR: Conceptualization, Funding Acquisition, Methodology, Writing - Original Draft, Supervision; JB: Conceptualization, Methodology, Writing - Original Draft, Supervision; All authors reviewed and approved the final manuscript.
Data availability statement
The datasets generated during this study are not publicly available due to confidentiality constraints but can be obtained from the corresponding author upon reasonable request.
Type of study: Original Article |
Subject:
Nursing
References
1. Nyelisani M, Makhado L, Luhalima T. A professional nurse's understanding of quality nursing care in Limpopo province, South Africa. curationis. 2023;46(1):2322. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Atashzadeh Shoorideh F, Pazargadi M, Zagheri Tafreshi M. The concept of nursing care quality from the perspective of stakeholders: a phenomenological study. J of Qual Res Health Sci. 2012;1(3):214-28. [View at Publisher] [Google Scholar]
3. Danno CH, Esteves LSF, Bohomol E. Quality improvement programs and the professional nursing practice environment: an integrative review. Rev Bras Enferm. 2021;74(1):e20200108. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Hickey JV, Giardino ER. The role of the nurse in quality improvement and patient safety. Pielęgniarstwo Neurologiczne i Neurochirurgiczne. 2019;8(1):30-6. [View at Publisher] [DOI] [Google Scholar]
5. Pires BSM, Oliveira LZFd, Siqueira CL, Feldman LB, Oliveira RA, Gasparino RC. Nurse work environment: comparison between private and public hospitals. Einstein (Sao Paulo). 2018;16(4):eAO4322. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Lu H, Zhao Y, While A. Job satisfaction among hospital nurses: A literature review. Int J Nurs Stud. 2019;94:21-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Endeshaw B. Healthcare service quality-measurement models: a review. Journal of Health Research. 2021;35(2):106-17. [View at Publisher] [DOI] [Google Scholar]
8. Moayed MS, Khalili R, Ebadi A, Parandeh A. Factors determining the quality of health services provided to COVID-19 patients from the perspective of healthcare providers: Based on the Donabedian model. Front Public Health. 2022;10:967431. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. ANCC. International Information for the Magnet Program 2023. [View at Publisher]
10. Lyle-Edrosolo G, Waxman K. Aligning healthcare safety and quality competencies: quality and safety education for nurses (QSEN), The Joint Commission, and American Nurses Credentialing Center (ANCC) magnet® standards crosswalk. Nurse Leader. 2016;14(1):70-5. [View at Publisher] [DOI] [Google Scholar]
11. Gordin P, Fields H. Operationalizing structural empowerment in a Magnet® organization 2020. [View at Publisher] [Google Scholar]
12. Kelly LA, McHugh MD, Aiken LH. Nurse outcomes in Magnet® and non-Magnet hospitals. J Nurs Adm. 2011;41(10):428-33. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Stone L, Arneil M, Coventry L, Casey V, Moss S, Cavadino A, et al. Benchmarking nurse outcomes in Australian Magnet® hospitals: cross-sectional survey. BMC nursing. 2019;18:62. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Negarandeh R. Facing nursing shortage: a complex challenge. Hayat. 2015;20(4):1-4. [View at Publisher] [Google Scholar]
15. Ghaleh EA, Farsani SJ, Ariamloo P, Mehrnoosh N, Rassouli M, Ebadi A. Patient education and follow-up units in Iran: A quality improvement project. Nursing Practice Today. 2024;12(1). [View at Publisher] [DOI] [Google Scholar]
16. Camila L. Empowering Patient Recovery: The Vitality of Hospital Nursing Care. J Nurs Care. 2024;13(1):635-40. [View at Publisher]
17. Alshammari SHS, Alfowais, FA, Al-Mutairi MGA, Aldhafeeri DD, Alshmmri FA, Khdhaier AM. The Effects of Hourly Rounding by Nursing Staff on Patient Safety and Satisfaction: Implications for Clinical Practice and Healthcare Administration. Journal of Ecohumanism. 2024;3(8):9406. [View at Publisher] [DOI] [Google Scholar]
18. Cornish F, Breton N, Moreno-Tabarez U, Delgado J, Rua M, de-Graft Aikins A, et al. Participatory action research. Nat Rev Methods Primers. 2023;3(1):34. [View at Publisher] [DOI] [Google Scholar]
19. Mohammadi M, Bergh A-M, Jahdi NS, Valizadeh L, Hosseini M, Hakimi S. Launching continuous kangaroo mother care through participatory action research in Iran. BMC Health Serv Res. 2023;23(1):436. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Ashrafizadeh H, Ebadi A, Rassouli M. The importance of paying attention to the Magnet Hospital project in Iran. Nursing Practice Today. 2024;11(2):89-91. [View at Publisher] [DOI] [Google Scholar]
21. Association AN. Magnet model: Creating a magnet culture. American Nurses Credentialing Center. 2017. [View at paplisher] [Google Scholar]
22. Svensson I, Bridges J, Ellis J, Brady N, Dello S, Hooft J, et al. Laying the foundations for implementing magnet principles in hospitals in Europe: a qualitative analysis. Int J Nurs Stud. 2024;154:104754. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Paquay M, Boulanger J-M, Locquet M, Dubois N, Ghuysen A. Exploring the feasibility of the Magnet Hospital concept within a European university nursing department: a mixed-methods study. Contemp Nurse. 2021;57(3-4):187-201. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Urden LD, Baclig JT, Sanchez K. A qualitative exploration of chief nursing officer perspectives on maintaining magnet® designation. J Nurs Adm.
2021;51(10):513-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Maier CB, Gurisch C, Köppen J, Kleine J, Aiken LH. Nurse‐sensitive quality and benchmarking in hospitals striving for Magnet® or Pathway® designation:A qualitative study. J Adv Nurs. 2024. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Abuzied Y, Al-Amer R, Abuzaid M, Somduth S. The magnet recognition program and quality improvement in nursing. Glob J Qual Saf Healthc. 2022;5(4):106-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Hidayah N, Arbianingsih, Ilham. The impact of integrated quality management-based health services on general hospital quality. Front Public Health. 2022;10:1011396. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Mabini Jr SP, Narsico LO, Narsico PG. Service quality, patient satisfaction, and improvement indicators. International Journal of Multidisciplinary: Applied Business and Education Research. 2024;5(4):1331-45. [View at Publisher] [DOI] [Google Scholar]
29. Askari R, Pishehvaran M, Arabi M. Investigating the Realization of Magnet Hospital Components in Educational Hospitals of Shahid Sadoughi University of Medical Sciences-Yazd. Evidence Based Health Policy, Management and Economics. 2020;4(3):189-96. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |